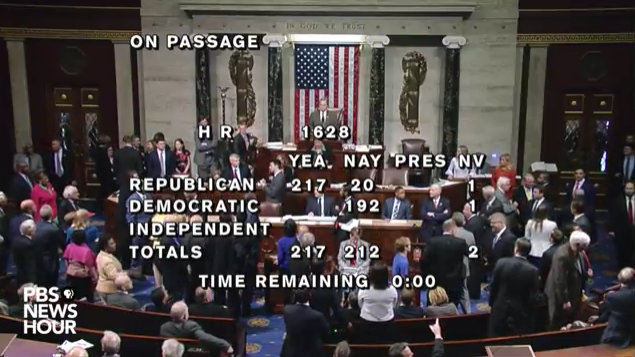
Washington, DC…The House Republicans narrowly advanced the “American Healthcare Act” on to the Senate. Many of the Obamacare mandates have been stripped in this bill including individual and employer mandates. The full text of the bill in its’ current form is below.
Union Calendar No. 30
115th CONGRESS
1st Session
H. R. 1628
[Report No. 115-52]
To provide for reconciliation pursuant to title II of the concurrent
resolution on the budget for fiscal year 2017.
_______________________________________________________________________
IN THE HOUSE OF REPRESENTATIVES
March 20, 2017
Mrs. Black from the Committee on the Budget, reported the following
bill; which was committed to the Committee of the Whole House on the
State of the Union and ordered to be printed
_______________________________________________________________________
A BILL
To provide for reconciliation pursuant to title II of the concurrent
resolution on the budget for fiscal year 2017.
Be it enacted by the Senate and House of Representatives of the
United States of America in Congress assembled,
SECTION 1. SHORT TITLE.
This Act may be cited as the “American Health Care Act of 2017”.
SEC. 2. TABLE OF CONTENTS.
The table of contents of this Act is as follows:
Sec. 1. Short title.
Sec. 2. Table of contents.
TITLE I–ENERGY AND COMMERCE
Subtitle A–Patient Access to Public Health Programs
Sec. 101. The Prevention and Public Health Fund.
Sec. 102. Community health center program.
Sec. 103. Federal payments to States.
Subtitle B–Medicaid Program Enhancement
Sec. 111. Repeal of Medicaid provisions.
Sec. 112. Repeal of Medicaid expansion.
Sec. 113. Elimination of DSH cuts.
Sec. 114. Reducing State Medicaid costs.
Sec. 115. Safety net funding for non-expansion States.
Sec. 116. Providing incentives for increased frequency of eligibility
redeterminations.
Subtitle C–Per Capita Allotment for Medical Assistance
Sec. 121. Per capita allotment for medical assistance.
Subtitle D–Patient Relief and Health Insurance Market Stability
Sec. 131. Repeal of cost-sharing subsidy.
Sec. 132. Patient and State Stability Fund.
Sec. 133. Continuous health insurance coverage incentive.
Sec. 134. Increasing coverage options.
Sec. 135. Change in permissible age variation in health insurance
premium rates.
TITLE II–COMMITTEE ON WAYS AND MEANS
Subtitle A–Repeal and Replace of Health-Related Tax Policy
Sec. 201. Recapture excess advance payments of premium tax credits.
Sec. 202. Additional modifications to premium tax credit.
Sec. 203. Premium tax credit.
Sec. 204. Small business tax credit.
Sec. 205. Individual mandate.
Sec. 206. Employer mandate.
Sec. 207. Repeal of the tax on employee health insurance premiums and
health plan benefits.
Sec. 208. Repeal of tax on over-the-counter medications.
Sec. 209. Repeal of increase of tax on health savings accounts.
Sec. 210. Repeal of limitations on contributions to flexible spending
accounts.
Sec. 211. Repeal of medical device excise tax.
Sec. 212. Repeal of elimination of deduction for expenses allocable to
medicare part D subsidy.
Sec. 213. Repeal of increase in income threshold for determining
medical care deduction.
Sec. 214. Repeal of Medicare tax increase.
Sec. 215. Refundable tax credit for health insurance coverage.
Sec. 216. Maximum contribution limit to health savings account
increased to amount of deductible and out-
of-pocket limitation.
Sec. 217. Allow both spouses to make catch-up contributions to the same
health savings account.
Sec. 218. Special rule for certain medical expenses incurred before
establishment of health savings account.
Subtitle B–Repeal of Certain Consumer Taxes
Sec. 221. Repeal of tax on prescription medications.
Sec. 222. Repeal of health insurance tax.
Subtitle C–Repeal of Tanning Tax
Sec. 231. Repeal of tanning tax.
Subtitle D–Remuneration From Certain Insurers
Sec. 241. Remuneration from certain insurers.
Subtitle E–Repeal of Net Investment Income Tax
Sec. 251. Repeal of net investment income tax.
TITLE I–ENERGY AND COMMERCE
Subtitle A–Patient Access to Public Health Programs
SEC. 101. THE PREVENTION AND PUBLIC HEALTH FUND.
(a) In General.–Subsection (b) of section 4002 of the Patient
Protection and Affordable Care Act (42 U.S.C. 300u-11), as amended by
section 5009 of the 21st Century Cures Act, is amended–
(1) in paragraph (2), by adding “and” at the end;
(2) in paragraph (3)–
(A) by striking “each of fiscal years 2018 and
2019” and inserting “fiscal year 2018”; and
(B) by striking the semicolon at the end and
inserting a period; and
(3) by striking paragraphs (4) through (8).
(b) Rescission of Unobligated Funds.–Of the funds made available
by such section 4002, the unobligated balance at the end of fiscal year
2018 is rescinded.
SEC. 102. COMMUNITY HEALTH CENTER PROGRAM.
Effective as if included in the enactment of the Medicare Access
and CHIP Reauthorization Act of 2015 (Public Law 114-10, 129 Stat. 87),
paragraph (1) of section 221(a) of such Act is amended by inserting “,
and an additional $422,000,000 for fiscal year 2017” after “2017”.
SEC. 103. FEDERAL PAYMENTS TO STATES.
(a) In General.–Notwithstanding section 504(a), 1902(a)(23),
1903(a), 2002, 2005(a)(4), 2102(a)(7), or 2105(a)(1) of the Social
Security Act (42 U.S.C. 704(a), 1396a(a)(23), 1396b(a), 1397a,
1397d(a)(4), 1397bb(a)(7), 1397ee(a)(1)), or the terms of any Medicaid
waiver in effect on the date of enactment of this Act that is approved
under section 1115 or 1915 of the Social Security Act (42 U.S.C. 1315,
1396n), for the 1-year period beginning on the date of the enactment of
this Act, no Federal funds provided from a program referred to in this
subsection that is considered direct spending for any year may be made
available to a State for payments to a prohibited entity, whether made
directly to the prohibited entity or through a managed care
organization under contract with the State.
(b) Definitions.–In this section:
(1) Prohibited entity.–The term “prohibited entity”
means an entity, including its affiliates, subsidiaries,
successors, and clinics–
(A) that, as of the date of enactment of this Act–
(i) is an organization described in section
501(c)(3) of the Internal Revenue Code of 1986
and exempt from tax under section 501(a) of
such Code;
(ii) is an essential community provider
described in section 156.235 of title 45, Code
of Federal Regulations (as in effect on the
date of enactment of this Act), that is
primarily engaged in family planning services,
reproductive health, and related medical care;
and
(iii) provides for abortions, other than an
abortion–
(I) if the pregnancy is the result
of an act of rape or incest; or
(II) in the case where a woman
suffers from a physical disorder,
physical injury, or physical illness
that would, as certified by a
physician, place the woman in danger of
death unless an abortion is performed,
including a life-endangering physical
condition caused by or arising from the
pregnancy itself; and
(B) for which the total amount of Federal and State
expenditures under the Medicaid program under title XIX
of the Social Security Act in fiscal year 2014 made
directly to the entity and to any affiliates,
subsidiaries, successors, or clinics of the entity, or
made to the entity and to any affiliates, subsidiaries,
successors, or clinics of the entity as part of a
nationwide health care provider network, exceeded
$350,000,000.
(2) Direct spending.–The term “direct spending” has the
meaning given that term under section 250(c) of the Balanced
Budget and Emergency Deficit Control Act of 1985 (2 U.S.C.
900(c)).
Subtitle B–Medicaid Program Enhancement
SEC. 111. REPEAL OF MEDICAID PROVISIONS.
The Social Security Act is amended–
(1) in section 1902 (42 U.S.C. 1396a)–
(A) in subsection (a)(47)(B), by inserting “and
provided that any such election shall cease to be
effective on January 1, 2020, and no such election
shall be made after that date” before the semicolon at
the end; and
(B) in subsection (l)(2)(C), by inserting “and
ending December 31, 2019,” after “January 1, 2014,”;
(2) in section 1915(k)(2) (42 U.S.C. 1396n(k)(2)), by
striking “during the period described in paragraph (1)” and
inserting “on or after the date referred to in paragraph (1)
and before January 1, 2020”; and
(3) in section 1920(e) (42 U.S.C. 1396r-1(e)), by striking
“under clause (i)(VIII), clause (i)(IX), or clause (ii)(XX) of
subsection (a)(10)(A)” and inserting “under clause (i)(VIII)
or clause (ii)(XX) of section 1902(a)(10)(A) before January 1,
2020, section 1902(a)(10)(A)(i)(IX),”.
SEC. 112. REPEAL OF MEDICAID EXPANSION.
(a) In General.–Section 1902(a)(10)(A) of the Social Security Act
(42 U.S.C. 1396a(a)(10)(A)) is amended–
(1) in clause (i)(VIII), by inserting “at the option of a
State,” after “January 1, 2014,”; and
(2) in clause (ii)(XX), by inserting “and ending December
31, 2019,” after “2014,”.
(b) Termination of EFMAP for New ACA Expansion Enrollees.–Section
1905 of the Social Security Act (42 U.S.C. 1396d) is amended–
(1) in subsection (y)(1), in the matter preceding
subparagraph (A), by striking “with respect to” and all that
follows through “shall be” and inserting “with respect to
amounts expended before January 1, 2020, by such State for
medical assistance for newly eligible individuals described in
subclause (VIII) of section 1902(a)(10)(A)(i) who are enrolled
under the State plan (or a waiver of the plan) before such date
and with respect to amounts expended after such date by such
State for medical assistance for individuals described in such
subclause who were enrolled under such plan (or waiver of such
plan) as of December 31, 2019, and who do not have a break in
eligibility for medical assistance under such State plan (or
waiver) for more than one month after such date, shall be”;
and
(2) in subsection (z)(2)–
(A) in subparagraph (A), by striking “medical
assistance for individuals” and all that follows
through “shall be” and inserting “amounts expended
before January 1, 2020, by such State for medical
assistance for individuals described in section
1902(a)(10)(A)(i)(VIII) who are nonpregnant childless
adults with respect to whom the State may require
enrollment in benchmark coverage under section 1937 and
who are enrolled under the State plan (or a waiver of
the plan) before such date and with respect to amounts
expended after such date by such State for medical
assistance for individuals described in such section,
who are nonpregnant childless adults with respect to
whom the State may require enrollment in benchmark
coverage under section 1937, who were enrolled under
such plan (or waiver of such plan) as of December 31,
2019, and who do not have a break in eligibility for
medical assistance under such State plan (or waiver)
for more than one month after such date, shall be”;
and
(B) in subparagraph (B)(ii)–
(i) in subclause (III), by adding “and”
at the end; and
(ii) by striking subclauses (IV), (V), and
(VI) and inserting the following new subclause:
“(IV) 2017 and each subsequent year is 80
percent.”.
(c) Sunset of Essential Health Benefits Requirement.–Section
1937(b)(5) of the Social Security Act (42 U.S.C. 1396u-7(b)(5)) is
amended by adding at the end the following: “This paragraph shall not
apply after December 31, 2019.”.
SEC. 113. ELIMINATION OF DSH CUTS.
Section 1923(f) of the Social Security Act (42 U.S.C. 1396r-4(f))
is amended–
(1) in paragraph (7)–
(A) in subparagraph (A)–
(i) in clause (i)–
(I) in the matter preceding
subclause (I), by striking “2025” and
inserting “2019”; and
(ii) in clause (ii)–
(I) in subclause (I), by adding
“and” at the end;
(II) in subclause (II), by striking
the semicolon at the end and inserting
a period; and
(III) by striking subclauses (III)
through (VIII); and
(B) by adding at the end the following new
subparagraph:
“(C) Exemption from exemption for non-expansion
states.–
“(i) In general.–In the case of a State
that is a non-expansion State for a fiscal
year, subparagraph (A)(i) shall not apply to
the DSH allotment for such State and fiscal
year.
“(ii) No change in reduction for expansion
states.–In the case of a State that is an
expansion State for a fiscal year, the DSH
allotment for such State and fiscal year shall
be determined as if clause (i) did not apply.
“(iii) Non-expansion and expansion state
defined.–
“(I) The term `expansion State’
means with respect to a fiscal year, a
State that, as of July 1 of the
preceding fiscal year, provides for
eligibility under clause (i)(VIII) or
(ii)(XX) of section 1902(a)(10)(A) for
medical assistance under this title (or
a waiver of the State plan approved
under section 1115).
“(II) The term `non-expansion
State’ means, with respect to a fiscal
year, a State that is not an expansion
State.”; and
(2) in paragraph (8), by striking “fiscal year 2025” and
inserting “fiscal year 2019”.
SEC. 114. REDUCING STATE MEDICAID COSTS.
(a) Letting States Disenroll High Dollar Lottery Winners.–
(1) In general.–Section 1902 of the Social Security Act
(42 U.S.C. 1396a) is amended–
(A) in subsection (a)(17), by striking “(e)(14),
(e)(14)” and inserting “(e)(14), (e)(15)”; and
(B) in subsection (e)–
(i) in paragraph (14) (relating to modified
adjusted gross income), by adding at the end
the following new subparagraph:
“(J) Treatment of certain lottery winnings and
income received as a lump sum.–
“(i) In general.–In the case of an
individual who is the recipient of qualified
lottery winnings (pursuant to lotteries
occurring on or after January 1, 2020) or
qualified lump sum income (received on or after
such date) and whose eligibility for medical
assistance is determined based on the
application of modified adjusted gross income
under subparagraph (A), a State shall, in
determining such eligibility, include such
winnings or income (as applicable) as income
received–
“(I) in the month in which such
winnings or income (as applicable) is
received if the amount of such winnings
or income is less than $80,000;
“(II) over a period of 2 months if
the amount of such winnings or income
(as applicable) is greater than or
equal to $80,000 but less than $90,000;
“(III) over a period of 3 months
if the amount of such winnings or
income (as applicable) is greater than
or equal to $90,000 but less than
$100,000; and
“(IV) over a period of 3 months
plus 1 additional month for each
increment of $10,000 of such winnings
or income (as applicable) received, not
to exceed a period of 120 months (for
winnings or income of $1,260,000 or
more), if the amount of such winnings
or income is greater than or equal to
$100,000.
“(ii) Counting in equal installments.–For
purposes of subclauses (II), (III), and (IV) of
clause (i), winnings or income to which such
subclause applies shall be counted in equal
monthly installments over the period of months
specified under such subclause.
“(iii) Hardship exemption.–An individual
whose income, by application of clause (i),
exceeds the applicable eligibility threshold
established by the State, may continue to be
eligible for medical assistance to the extent
that the State determines, under procedures
established by the State under the State plan
(or in the case of a waiver of the plan under
section 1115, incorporated in such waiver), or
as otherwise established by such State in
accordance with such standards as may be
specified by the Secretary, that the denial of
eligibility of the individual would cause an
undue medical or financial hardship as
determined on the basis of criteria established
by the Secretary.
“(iv) Notifications and assistance
required in case of loss of eligibility.–A
State shall, with respect to an individual who
loses eligibility for medical assistance under
the State plan (or a waiver of such plan) by
reason of clause (i), before the date on which
the individual loses such eligibility, inform
the individual of the date on which the
individual would no longer be considered
ineligible by reason of such clause to receive
medical assistance under the State plan or
under any waiver of such plan and the date on
which the individual would be eligible to
reapply to receive such medical assistance.
“(v) Qualified lottery winnings defined.–
In this subparagraph, the term `qualified
lottery winnings’ means winnings from a
sweepstakes, lottery, or pool described in
paragraph (3) of section 4402 of the Internal
Revenue Code of 1986 or a lottery operated by a
multistate or multijurisdictional lottery
association, including amounts awarded as a
lump sum payment.
“(vi) Qualified lump sum income defined.–
In this subparagraph, the term `qualified lump
sum income’ means income that is received as a
lump sum from one of the following sources:
“(I) Monetary winnings from
gambling (as defined by the Secretary
and including monetary winnings from
gambling activities described in
section 1955(b)(4) of title 18, United
States Code).
“(II) Income received as liquid
assets from the estate (as defined in
section 1917(b)(4)) of a deceased
individual.”; and
(ii) by striking “(14) Exclusion” and
inserting “(15) Exclusion”.
(2) Rules of construction.–
(A) Interception of lottery winnings allowed.–
Nothing in the amendment made by paragraph (1)(B)(i)
shall be construed as preventing a State from
intercepting the State lottery winnings awarded to an
individual in the State to recover amounts paid by the
State under the State Medicaid plan under title XIX of
the Social Security Act for medical assistance
furnished to the individual.
(B) Applicability limited to eligibility of
recipient of lottery winnings or lump sum income.–
Nothing in the amendment made by paragraph (1)(B)(i)
shall be construed, with respect to a determination of
household income for purposes of a determination of
eligibility for medical assistance under the State plan
under title XIX of the Social Security Act (42 U.S.C.
1396 et seq.) (or a waiver of such plan) made by
applying modified adjusted gross income under
subparagraph (A) of section 1902(e)(14) of such Act (42
U.S.C. 1396a(e)(14)), as limiting the eligibility for
such medical assistance of any individual that is a
member of the household other than the individual (or
the individual’s spouse) who received qualified lottery
winnings or qualified lump-sum income (as defined in
subparagraph (J) of such section 1902(e)(14), as added
by paragraph (1)(B)(i) of this subsection).
(b) Repeal of Retroactive Eligibility.–
(1) In general.–
(A) State plan requirements.–Section 1902(a)(34)
of the Social Security Act (42 U.S.C. 1396a(a)(34)) is
amended by striking “in or after the third month
before the month in which he made application” and
inserting “in or after the month in which the
individual made application”.
(B) Definition of medical assistance.–Section
1905(a) of the Social Security Act (42 U.S.C. 1396d(a))
is amended by striking “in or after the third month
before the month in which the recipient makes
application for assistance” and inserting “in or
after the month in which the recipient makes
application for assistance”.
(2) Effective date.–The amendments made by paragraph (1)
shall apply to medical assistance with respect to individuals
whose eligibility for such assistance is based on an
application for such assistance made (or deemed to be made) on
or after October 1, 2017.
(c) Ensuring States Are Not Forced to Pay for Individuals
Ineligible for the Program.–
(1) In general.–Section 1137(f) of the Social Security Act
(42 U.S.C. 1320b-7(f)) is amended–
(A) by striking “Subsections (a)(1) and (d)” and
inserting “(1) Subsections (a)(1) and (d)”; and
(B) by adding at the end the following new
paragraph:
“(2)(A) Subparagraphs (A) and (B)(ii) of subsection (d)(4) shall
not apply in the case of an initial determination made on or after the
date that is 6 months after the date of the enactment of this paragraph
with respect to the eligibility of an alien described in subparagraph
(B) for benefits under the program listed in subsection (b)(2).
“(B) An alien described in this subparagraph is an individual
declaring to be a citizen or national of the United States with respect
to whom a State, in accordance with section 1902(a)(46)(B), requires–
“(i) pursuant to 1902(ee), the submission of a social
security number; or
“(ii) pursuant to 1903(x), the presentation of
satisfactory documentary evidence of citizenship or
nationality.”.
(2) No payments for medical assistance provided before
presentation of evidence.–Section 1903(i)(22) of the Social
Security Act (42 U.S.C. 1396b(i)(22)) is amended–
(A) by striking “with respect to amounts
expended” and inserting “(A) with respect to amounts
expended”;
(B) by inserting “and” at the end; and
(C) by adding at the end the following new
subparagraph:
“(B) in the case of a State that elects to provide a
reasonable period to present satisfactory documentary evidence
of such citizenship or nationality pursuant to paragraph (2)(C)
of section 1902(ee) or paragraph (4) of subsection (x) of this
section, for amounts expended for medical assistance for such
an individual (other than an individual described in paragraph
(2) of such subsection (x)) during such period;”.
(3) Conforming amendments.–Section 1137(d)(4) of the
Social Security Act (42 U.S.C. 1320b-7(d)(4)) is amended–
(A) in subparagraph (A), in the matter preceding
clause (i), by inserting “subject to subsection
(f)(2),” before “the State”; and
(B) in subparagraph (B)(ii), by inserting “subject
to subsection (f)(2),” before “pending such
verification”.
(d) Updating Allowable Home Equity Limits in Medicaid.–
(1) In general.–Section 1917(f)(1) of the Social Security
Act (42 U.S.C. 1396p(f)(1)) is amended–
(A) in subparagraph (A), by striking
“subparagraphs (B) and (C)” and inserting
“subparagraph (B)”;
(B) by striking subparagraph (B);
(C) by redesignating subparagraph (C) as
subparagraph (B); and
(D) in subparagraph (B), as so redesignated, by
striking “dollar amounts specified in this paragraph”
and inserting “dollar amount specified in subparagraph
(A)”.
(2) Effective date.–
(A) In general.–The amendments made by paragraph
(1) shall apply with respect to eligibility
determinations made after the date that is 180 days
after the date of the enactment of this section.
(B) Exception for state legislation.–In the case
of a State plan under title XIX of the Social Security
Act that the Secretary of Health and Human Services
determines requires State legislation in order for the
respective plan to meet any requirement imposed by
amendments made by this subsection, the respective plan
shall not be regarded as failing to comply with the
requirements of such title solely on the basis of its
failure to meet such an additional requirement before
the first day of the first calendar quarter beginning
after the close of the first regular session of the
State legislature that begins after the date of the
enactment of this Act. For purposes of the previous
sentence, in the case of a State that has a 2-year
legislative session, each year of the session shall be
considered to be a separate regular session of the
State legislature.
SEC. 115. SAFETY NET FUNDING FOR NON-EXPANSION STATES.
Title XIX of the Social Security Act is amended by inserting after
section 1923 (42 U.S.C. 1396r-4) the following new section:
“adjustment in payment for services of safety net providers in non-
expansion states
“Sec. 1923A. (a) In General.–Subject to the limitations of this
section, for each year during the period beginning with 2018 and ending
with 2021, each State that is one of the 50 States or the District of
Columbia and that, as of July 1 of the preceding year, did not provide
for eligibility under clause (i)(VIII) or (ii)(XX) of section
1902(a)(10)(A) for medical assistance under this title (or a waiver of
the State plan approved under section 1115) (each such State or
District referred to in this section for the year as a `non-expansion
State’) may adjust the payment amounts otherwise provided under the
State plan under this title (or a waiver of such plan) to health care
providers that provide health care services to individuals enrolled
under this title (in this section referred to as `eligible providers’).
“(b) Increase in Applicable FMAP.–Notwithstanding section
1905(b), the Federal medical assistance percentage applicable with
respect to expenditures attributable to a payment adjustment under
subsection (a) for which payment is permitted under subsection (c)
shall be equal to–
“(1) 100 percent for calendar quarters in calendar years
2018, 2019, 2020, and 2021; and
“(2) 95 percent for calendar quarters in calendar year
2022.
“(c) Limitations; Disqualification of States.–
“(1) Annual allotment limitation.–Payment under section
1903(a) shall not be made to a State with respect to any
payment adjustment made under this section for all calendar
quarters in a year in excess of the $2,000,000,000 multiplied
by the ratio of–
“(A) the population of the State with income below
138 percent of the poverty line in 2015 (as determined
based the table entitled `Health Insurance Coverage
Status and Type by Ratio of Income to Poverty Level in
the Past 12 Months by Age’ for the universe of the
civilian noninstitutionalized population for whom
poverty status is determined based on the 2015 American
Community Survey 1-Year Estimates, as published by the
Bureau of the Census), to
“(B) the sum of the populations under subparagraph
(A) for all non-expansion States.
“(2) Limitation on payment adjustment amount for
individual providers.–The amount of a payment adjustment under
subsection (a) for an eligible provider may not exceed the
provider’s costs incurred in furnishing health care services
(as determined by the Secretary and net of payments under this
title, other than under this section, and by uninsured
patients) to individuals who either are eligible for medical
assistance under the State plan (or under a waiver of such
plan) or have no health insurance or health plan coverage for
such services.
“(d) Disqualification in Case of State Coverage Expansion.–If a
State is a non-expansion for a year and provides eligibility for
medical assistance described in subsection (a) during the year, the
State shall no longer be treated as a non-expansion State under this
section for any subsequent years.”.
SEC. 116. PROVIDING INCENTIVES FOR INCREASED FREQUENCY OF ELIGIBILITY
REDETERMINATIONS.
(a) In General.–Section 1902(e)(14) of the Social Security Act (42
U.S.C. 1396a(e)(14)) (relating to modified adjusted gross income), as
amended by section 114(a)(1), is further amended by adding at the end
the following:
“(K) Frequency of eligibility redeterminations.–
Beginning on October 1, 2017, and notwithstanding
subparagraph (H), in the case of an individual whose
eligibility for medical assistance under the State plan
under this title (or a waiver of such plan) is
determined based on the application of modified
adjusted gross income under subparagraph (A) and who is
so eligible on the basis of clause (i)(VIII) or clause
(ii)(XX) of subsection (a)(10)(A), a State shall
redetermine such individual’s eligibility for such
medical assistance no less frequently than once every 6
months.”.
(b) Civil Monetary Penalty.–Section 1128A(a) of the Social
Security Act (42 U.S.C. 1320a-7a(a)) is amended, in the matter
following paragraph (10), by striking “(or, in cases under paragraph
(3)” and inserting the following: “(or, in cases under paragraph (1)
in which an individual was knowingly enrolled on or after October 1,
2017, pursuant to section 1902(a)(10)(A)(i)(VIII) for medical
assistance under the State plan under title XIX whose income does not
meet the income threshold specified in such section or in which a claim
was presented on or after October 1, 2017, as a claim for an item or
service furnished to an individual described in such section but whose
enrollment under such State plan is not made on the basis of such
individual’s meeting the income threshold specified in such section,
$20,000 for each such individual or claim; in cases under paragraph
(3)”.
(c) Increased Administrative Matching Percentage.–For each
calendar quarter during the period beginning on October 1, 2017, and
ending on December 31, 2019, the Federal matching percentage otherwise
applicable under section 1903(a) of the Social Security Act (42 U.S.C.
1396b(a)) with respect to State expenditures during such quarter that
are attributable to meeting the requirement of section 1902(e)(14)
(relating to determinations of eligibility using modified adjusted
gross income) of such Act shall be increased by 5 percentage points
with respect to State expenditures attributable to activities carried
out by the State (and approved by the Secretary) to increase the
frequency of eligibility redeterminations required by subparagraph (K)
of such section (relating to eligibility redeterminations made on a 6-
month basis) (as added by subsection (a)).
Subtitle C–Per Capita Allotment for Medical Assistance
SEC. 121. PER CAPITA ALLOTMENT FOR MEDICAL ASSISTANCE.
Title XIX of the Social Security Act is amended–
(1) in section 1903 (42 U.S.C. 1396b)–
(A) in subsection (a), in the matter before
paragraph (1), by inserting “and section 1903A(a)”
after “except as otherwise provided in this section”;
and
(B) in subsection (d)(1), by striking “to which”
and inserting “to which, subject to section
1903A(a),”; and
(2) by inserting after such section 1903 the following new
section:
“SEC. 1903A. PER CAPITA-BASED CAP ON PAYMENTS FOR MEDICAL ASSISTANCE.
“(a) Application of Per Capita Cap on Payments for Medical
Assistance Expenditures.–
“(1) In general.–If a State has excess aggregate medical
assistance expenditures (as defined in paragraph (2)) for a
fiscal year (beginning with fiscal year 2020), the amount of
payment to the State under section 1903(a)(1) for each quarter
in the following fiscal year shall be reduced by \1/4\ of the
excess aggregate medical assistance payments (as defined in
paragraph (3)) for that previous fiscal year. In this section,
the term `State’ means only the 50 States and the District of
Columbia.
“(2) Excess aggregate medical assistance expenditures.–In
this subsection, the term `excess aggregate medical assistance
expenditures’ means, for a State for a fiscal year, the amount
(if any) by which–
“(A) the amount of the adjusted total medical
assistance expenditures (as defined in subsection
(b)(1)) for the State and fiscal year; exceeds
“(B) the amount of the target total medical
assistance expenditures (as defined in subsection (c))
for the State and fiscal year.
“(3) Excess aggregate medical assistance payments.–In
this subsection, the term `excess aggregate medical assistance
payments’ means, for a State for a fiscal year, the product
of–
“(A) the excess aggregate medical assistance
expenditures (as defined in paragraph (2)) for the
State for the fiscal year; and
“(B) the Federal average medical assistance
matching percentage (as defined in paragraph (4)) for
the State for the fiscal year.
“(4) Federal average medical assistance matching
percentage.–In this subsection, the term `Federal average
medical assistance matching percentage’ means, for a State for
a fiscal year, the ratio (expressed as a percentage) of–
“(A) the amount of the Federal payments that would
be made to the State under section 1903(a)(1) for
medical assistance expenditures for calendar quarters
in the fiscal year if paragraph (1) did not apply; to
“(B) the amount of the medical assistance
expenditures for the State and fiscal year.
“(b) Adjusted Total Medical Assistance Expenditures.–Subject to
subsection (g), the following shall apply:
“(1) In general.–In this section, the term `adjusted
total medical assistance expenditures’ means, for a State–
“(A) for fiscal year 2016, the product of–
“(i) the amount of the medical assistance
expenditures (as defined in paragraph (2)) for
the State and fiscal year, reduced by the
amount of any excluded expenditures (as defined
in paragraph (3)) for the State and fiscal year
otherwise included in such medical assistance
expenditures; and
“(ii) the 1903A FY16 population percentage
(as defined in paragraph (4)) for the State; or
“(B) for fiscal year 2019 or a subsequent fiscal
year, the amount of the medical assistance expenditures
(as defined in paragraph (2)) for the State and fiscal
year that is attributable to 1903A enrollees, reduced
by the amount of any excluded expenditures (as defined
in paragraph (3)) for the State and fiscal year
otherwise included in such medical assistance
expenditures.
“(2) Medical assistance expenditures.–In this section,
the term `medical assistance expenditures’ means, for a State
and fiscal year, the medical assistance payments as reported by
medical service category on the Form CMS-64 quarterly expense
report (or successor to such a report form, and including
enrollment data and subsequent adjustments to any such report,
in this section referred to collectively as a `CMS-64 report’)
that directly result from providing medical assistance under
the State plan (including under a waiver of the plan) for which
payment is (or may otherwise be) made pursuant to section
1903(a)(1).
“(3) Excluded expenditures.–In this section, the term
`excluded expenditures’ means, for a State and fiscal year,
expenditures under the State plan (or under a waiver of such
plan) that are attributable to any of the following:
“(A) DSH.–Payment adjustments made for
disproportionate share hospitals under section 1923.
“(B) Medicare cost-sharing.–Payments made for
medicare cost-sharing (as defined in section
1905(p)(3)).
“(C) Safety net provider payment adjustments in
non-expansion states.–Payment adjustments under
subsection (a) of section 1923A for which payment is
permitted under subsection (c) of such section.
“(4) 1903A fy 16 population percentage.–In this
subsection, the term `1903A FY16 population percentage’ means,
for a State, the Secretary’s calculation of the percentage of
the actual medical assistance expenditures, as reported by the
State on the CMS-64 reports for calendar quarters in fiscal
year 2016, that are attributable to 1903A enrollees (as defined
in subsection (e)(1)).
“(c) Target Total Medical Assistance Expenditures.–
“(1) Calculation.–In this section, the term `target total
medical assistance expenditures’ means, for a State for a
fiscal year, the sum of the products, for each of the 1903A
enrollee categories (as defined in subsection (e)(2)), of–
“(A) the target per capita medical assistance
expenditures (as defined in paragraph (2)) for the
enrollee category, State, and fiscal year; and
“(B) the number of 1903A enrollees for such
enrollee category, State, and fiscal year, as
determined under subsection (e)(4).
“(2) Target per capita medical assistance expenditures.–
In this subsection, the term `target per capita medical
assistance expenditures’ means, for a 1903A enrollee category,
State, and a fiscal year, an amount equal to–
“(A) the provisional FY19 target per capita amount
for such enrollee category (as calculated under
subsection (d)(5)) for the State; increased by
“(B) the percentage increase in the medical care
component of the consumer price index for all urban
consumers (U.S. city average) from September of 2019 to
September of the fiscal year involved.
“(d) Calculation of FY19 Provisional Target Amount for Each 1903A
Enrollee Category.–Subject to subsection (g), the following shall
apply:
“(1) Calculation of base amounts for fiscal year 2016.–
For each State the Secretary shall calculate (and provide
notice to the State not later than April 1, 2018, of) the
following:
“(A) The amount of the adjusted total medical
assistance expenditures (as defined in subsection
(b)(1)) for the State for fiscal year 2016.
“(B) The number of 1903A enrollees for the State
in fiscal year 2016 (as determined under subsection
(e)(4)).
“(C) The average per capita medical assistance
expenditures for the State for fiscal year 2016 equal
to–
“(i) the amount calculated under
subparagraph (A); divided by
“(ii) the number calculated under
subparagraph (B).
“(2) Fiscal year 2019 average per capita amount based on
inflating the fiscal year 2016 amount to fiscal year 2019 by
cpi-medical.–The Secretary shall calculate a fiscal year 2019
average per capita amount for each State equal to–
“(A) the average per capita medical assistance
expenditures for the State for fiscal year 2016
(calculated under paragraph (1)(C)); increased by
“(B) the percentage increase in the medical care
component of the consumer price index for all urban
consumers (U.S. city average) from September, 2016 to
September, 2019.
“(3) Aggregate and average expenditures per capita for
fiscal year 2019.–The Secretary shall calculate for each State
the following:
“(A) The amount of the adjusted total medical
assistance expenditures (as defined in subsection
(b)(1)) for the State for fiscal year 2019.
“(B) The number of 1903A enrollees for the State
in fiscal year 2019 (as determined under subsection
(e)(4)).
“(4) Per capita expenditures for fiscal year 2019 for each
1903a enrollee category.–The Secretary shall calculate (and
provide notice to each State not later than January 1, 2020,
of) the following:
“(A)(i) For each 1903A enrollee category, the
amount of the adjusted total medical assistance
expenditures (as defined in subsection (b)(1)) for the
State for fiscal year 2019 for individuals in the
enrollee category, calculated by excluding from medical
assistance expenditures those expenditures attributable
to expenditures described in clause (iii) or non-DSH
supplemental expenditures (as defined in clause (ii)).
“(ii) In this paragraph, the term `non-DSH
supplemental expenditure’ means a payment to a provider
under the State plan (or under a waiver of the plan)
that–
“(I) is not made under section 1923;
“(II) is not made with respect to a
specific item or service for an individual;
“(III) is in addition to any payments made
to the provider under the plan (or waiver) for
any such item or service; and
“(IV) complies with the limits for
additional payments to providers under the plan
(or waiver) imposed pursuant to section
1902(a)(30)(A), including the regulations
specifying upper payment limits under the State
plan in part 447 of title 42, Code of Federal
Regulations (or any successor regulations).
“(iii) An expenditure described in this clause is
an expenditure that meets the criteria specified in
subclauses (I), (II), and (III) of clause (ii) and is
authorized under section 1115 for the purposes of
funding a delivery system reform pool, uncompensated
care pool, a designated state health program, or any
other similar expenditure (as defined by the
Secretary).
“(B) For each 1903A enrollee category, the number
of 1903A enrollees for the State in fiscal year 2019 in
the enrollee category (as determined under subsection
(e)(4)).
“(C) For fiscal year 2016, the State’s non-DSH
supplemental payment percentage is equal to the ratio
(expressed as a percentage) of–
“(i) the total amount of non-DSH
supplemental expenditures (as defined in
subparagraph (A)(ii)) for the State for fiscal
year 2016; to
“(ii) the amount described in subsection
(b)(1)(A) for the State for fiscal year 2016.
“(D) For each 1903A enrollee category an average
medical assistance expenditures per capita for the
State for fiscal year 2019 for the enrollee category
equal to–
“(i) the amount calculated under
subparagraph (A) for the State, increased by
the non-DSH supplemental payment percentage for
the State (as calculated under subparagraph
(C)); divided by
“(ii) the number calculated under
subparagraph (B) for the State for the enrollee
category.
“(5) Provisional fy19 per capita target amount for each
1903a enrollee category.–Subject to subsection (f)(2), the
Secretary shall calculate for each State a provisional FY19 per
capita target amount for each 1903A enrollee category equal to
the average medical assistance expenditures per capita for the
State for fiscal year 2019 (as calculated under paragraph
(4)(D)) for such enrollee category multiplied by the ratio of–
“(A) the product of–
“(i) the fiscal year 2019 average per
capita amount for the State, as calculated
under paragraph (2); and
“(ii) the number of 1903A enrollees for
the State in fiscal year 2019, as calculated
under paragraph (3)(B); to
“(B) the amount of the adjusted total medical
assistance expenditures for the State for fiscal year
2019, as calculated under paragraph (3)(A).
“(e) 1903A Enrollee; 1903A Enrollee Category.–Subject to
subsection (g), for purposes of this section, the following shall
apply:
“(1) 1903A enrollee.–The term `1903A enrollee’ means,
with respect to a State and a month, any Medicaid enrollee (as
defined in paragraph (3)) for the month, other than such an
enrollee who for such month is in any of the following
categories of excluded individuals:
“(A) CHIP.–An individual who is provided, under
this title in the manner described in section
2101(a)(2), child health assistance under title XXI.
“(B) IHS.–An individual who receives any medical
assistance under this title for services for which
payment is made under the third sentence of section
1905(b).
“(C) Breast and cervical cancer services eligible
individual.–An individual who is entitled to medical
assistance under this title only pursuant to section
1902(a)(10)(A)(ii)(XVIII).
“(D) Partial-benefit enrollees.–An individual
who–
“(i) is an alien who is entitled to
medical assistance under this title only
pursuant to section 1903(v)(2);
“(ii) is entitled to medical assistance
under this title only pursuant to subclause
(XII) or (XXI) of section 1902(a)(10)(A)(ii)
(or pursuant to a waiver that provides only
comparable benefits);
“(iii) is a dual eligible individual (as
defined in section 1915(h)(2)(B)) and is
entitled to medical assistance under this title
(or under a waiver) only for some or all of
medicare cost-sharing (as defined in section
1905(p)(3)); or
“(iv) is entitled to medical assistance
under this title and for whom the State is
providing a payment or subsidy to an employer
for coverage of the individual under a group
health plan pursuant to section 1906 or section
1906A (or pursuant to a waiver that provides
only comparable benefits).
“(2) 1903A enrollee category.–The term `1903A enrollee
category’ means each of the following:
“(A) Elderly.–A category of 1903A enrollees who
are 65 years of age or older.
“(B) Blind and disabled.–A category of 1903A
enrollees (not described in the previous subparagraph)
who are eligible for medical assistance under this
title on the basis of being blind or disabled.
“(C) Children.–A category of 1903A enrollees (not
described in a previous subparagraph) who are children
under 19 years of age.
“(D) Expansion enrollees.–A category of 1903A
enrollees (not described in a previous subparagraph)
for whom the amounts expended for medical assistance
are subject to an increase or change in the Federal
medical assistance percentage under subsection (y) or
(z)(2), respectively, of section 1905.
“(E) Other nonelderly, nondisabled, non-expansion
adults.–A category of 1903A enrollees who are not
described in any previous subparagraph.
“(3) Medicaid enrollee.–The term `Medicaid enrollee’
means, with respect to a State for a month, an individual who
is eligible for medical assistance for items or services under
this title and enrolled under the State plan (or a waiver of
such plan) under this title for the month.
“(4) Determination of number of 1903a enrollees.–The
number of 1903A enrollees for a State and fiscal year, and, if
applicable, for a 1903A enrollee category, is the average
monthly number of Medicaid enrollees for such State and fiscal
year (and, if applicable, in such category) that are reported
through the CMS-64 report under (and subject to audit under)
subsection (h).
“(f) Special Payment Rules.–
“(1) Application in case of research and demonstration
projects and other waivers.–In the case of a State with a
waiver of the State plan approved under section 1115, section
1915, or another provision of this title, this section shall
apply to medical assistance expenditures and medical assistance
payments under the waiver, in the same manner as if such
expenditures and payments had been made under a State plan
under this title and the limitations on expenditures under this
section shall supersede any other payment limitations or
provisions (including limitations based on a per capita
limitation) otherwise applicable under such a waiver.
“(2) Treatment of states expanding coverage after fiscal
year 2016.–In the case of a State that did not provide for
medical assistance for the 1903A enrollee category described in
subsection (e)(2)(D) during fiscal year 2016 but which provides
for such assistance for such category in a subsequent year, the
provisional FY19 per capita target amount for such enrollee
category under subsection (d)(5) shall be equal to the
provisional FY19 per capita target amount for the 1903A
enrollee category described in subsection (e)(2)(E).
“(3) In case of state failure to report necessary data.–
If a State for any quarter in a fiscal year (beginning with
fiscal year 2019) fails to satisfactorily submit data on
expenditures and enrollees in accordance with subsection
(h)(1), for such fiscal year and any succeeding fiscal year for
which such data are not satisfactorily submitted–
“(A) the Secretary shall calculate and apply
subsections (a) through (e) with respect to the State
as if all 1903A enrollee categories for which such
expenditure and enrollee data were not satisfactorily
submitted were a single 1903A enrollee category; and
“(B) the growth factor otherwise applied under
subsection (c)(2)(B) shall be decreased by 1 percentage
point.
“(g) Recalculation of Certain Amounts for Data Errors.–The
amounts and percentage calculated under paragraphs (1) and (4)(C) of
subsection (d) for a State for fiscal year 2016, and the amounts of the
adjusted total medical assistance expenditures calculated under
subsection (b) and the number of Medicaid enrollees and 1903A enrollees
determined under subsection (e)(4) for a State for fiscal year 2016,
fiscal year 2019, and any subsequent fiscal year, may be adjusted by
the Secretary based upon an appeal (filed by the State in such a form,
manner, and time, and containing such information relating to data
errors that support such appeal, as the Secretary specifies) that the
Secretary determines to be valid, except that any adjustment by the
Secretary under this subsection for a State may not result in an
increase of the target total medical assistance expenditures exceeding
2 percent.
“(h) Required Reporting and Auditing of CMS-64 Data; Transitional
Increase in Federal Matching Percentage for Certain Administrative
Expenses.–
“(1) Reporting.–In addition to the data required on form
Group VIII on the CMS-64 report form as of January 1, 2017, in
each CMS-64 report required to be submitted (for each quarter
beginning on or after October 1, 2018), the State shall include
data on medical assistance expenditures within such categories
of services and categories of enrollees (including each 1903A
enrollee category and each category of excluded individuals
under subsection (e)(1)) and the numbers of enrollees within
each of such enrollee categories, as the Secretary determines
are necessary (including timely guidance published as soon as
possible after the date of the enactment of this section) in
order to implement this section and to enable States to comply
with the requirement of this paragraph on a timely basis.
“(2) Auditing.–The Secretary shall conduct for each State
an audit of the number of individuals and expenditures reported
through the CMS-64 report for fiscal year 2016, fiscal year
2019, and each subsequent fiscal year, which audit may be
conducted on a representative sample (as determined by the
Secretary).
“(3) Temporary increase in federal matching percentage to
support improved data reporting systems for fiscal years 2018
and 2019.–For amounts expended during calendar quarters
beginning on or after October 1, 2017, and before October 1,
2019–
“(A) the Federal matching percentage applied under
section 1903(a)(3)(A)(i) shall be increased by 10
percentage points to 100 percent;
“(B) the Federal matching percentage applied under
section 1903(a)(3)(B) shall be increased by 25
percentage points to 100 percent; and
“(C) the Federal matching percentage applied under
section 1903(a)(7) shall be increased by 10 percentage
points to 60 percent but only with respect to amounts
expended that are attributable to a State’s additional
administrative expenditures to implement the data
requirements of paragraph (1).”.
Subtitle D–Patient Relief and Health Insurance Market Stability
SEC. 131. REPEAL OF COST-SHARING SUBSIDY.
(a) In General.–Section 1402 of the Patient Protection and
Affordable Care Act is repealed.
(b) Effective Date.–The repeal made by subsection (a) shall apply
to cost-sharing reductions (and payments to issuers for such
reductions) for plan years beginning after December 31, 2019.
SEC. 132. PATIENT AND STATE STABILITY FUND.
The Social Security Act (42 U.S.C. 301 et seq.) is amended by
adding at the end the following new title:
“TITLE XXII–PATIENT AND STATE STABILITY FUND
“SEC. 2201. ESTABLISHMENT OF PROGRAM.
“There is hereby established the `Patient and State Stability
Fund’ to be administered by the Secretary of Health and Human Services,
acting through the Administrator of the Centers for Medicare & Medicaid
Services (in this section referred to as the `Administrator’), to
provide funding, in accordance with this title, to the 50 States and
the District of Columbia (each referred to in this section as a
`State’) during the period, subject to section 2204(c), beginning on
January 1, 2018, and ending on December 31, 2026, for the purposes
described in section 2202.
“SEC. 2202. USE OF FUNDS.
“A State may use the funds allocated to the State under this title
for any of the following purposes:
“(1) Helping, through the provision of financial
assistance, high-risk individuals who do not have access to
health insurance coverage offered through an employer enroll in
health insurance coverage in the individual market in the
State, as such market is defined by the State (whether through
the establishment of a new mechanism or maintenance of an
existing mechanism for such purpose).
“(2) Providing incentives to appropriate entities to enter
into arrangements with the State to help stabilize premiums for
health insurance coverage in the individual market, as such
markets are defined by the State.
“(3) Reducing the cost for providing health insurance
coverage in the individual market and small group market, as
such markets are defined by the State, to individuals who have,
or are projected to have, a high rate of utilization of health
services (as measured by cost).
“(4) Promoting participation in the individual market and
small group market in the State and increasing health insurance
options available through such market.
“(5) Promoting access to preventive services; dental care
services (whether preventive or medically necessary); vision
care services (whether preventive or medically necessary);
prevention, treatment, or recovery support services for
individuals with mental or substance use disorders; or any
combination of such services.
“(6) Providing payments, directly or indirectly, to health
care providers for the provision of such health care services
as are specified by the Administrator.
“(7) Providing assistance to reduce out-of-pocket costs,
such as copayments, coinsurance, premiums, and deductibles, of
individuals enrolled in health insurance coverage in the State.
“SEC. 2203. STATE ELIGIBILITY AND APPROVAL; DEFAULT SAFEGUARD.
“(a) Encouraging State Options for Allocations.–
“(1) In general.–To be eligible for an allocation of
funds under this title for a year during the period described
in section 2201 for use for one or more purposes described in
section 2202, a State shall submit to the Administrator an
application at such time (but, in the case of allocations for
2018, not later than 45 days after the date of the enactment of
this title and, in the case of allocations for a subsequent
year, not later than March 31 of the previous year) and in such
form and manner as specified by the Administrator and
containing–
“(A) a description of how the funds will be used
for such purposes;
“(B) a certification that the State will make,
from non-Federal funds, expenditures for such purposes
in an amount that is not less than the State percentage
required for the year under section 2204(e)(1); and
“(C) such other information as the Administrator
may require.
“(2) Automatic approval.–An application so submitted is
approved unless the Administrator notifies the State submitting
the application, not later than 60 days after the date of the
submission of such application, that the application has been
denied for not being in compliance with any requirement of this
title and of the reason for such denial.
“(3) One-time application.–If an application of a State
is approved for a year, with respect to a purpose described in
section 2202, such application shall be treated as approved,
with respect to such purpose, for each subsequent year through
2026.
“(4) Treatment as a state health care program.–Any
program receiving funds from an allocation for a State under
this title, including pursuant to subsection (b), shall be
considered to be a `State health care program’ for purposes of
sections 1128, 1128A, and 1128B.
“(b) Default Federal Safeguard.–
“(1) In general.–
“(A) 2018.–For allocations made under this title
for 2018, in the case of a State that does not submit
an application under subsection (a) by the 45-day
submission date applicable to such year under
subsection (a)(1) and in the case of a State that does
submit such an application by such date that is not
approved, subject to section 2204(e), the
Administrator, in consultation with the State insurance
commissioner, shall use the allocation that would
otherwise be provided to the State under this title for
such year, in accordance with paragraph (2), for such
State.
“(B) 2019 through 2026.–In the case of a State
that does not have in effect an approved application
under this section for 2019 or a subsequent year
beginning during the period described in section 2201,
subject to section 2204(e), the Administrator, in
consultation with the State insurance commissioner,
shall use the allocation that would otherwise be
provided to the State under this title for such year,
in accordance with paragraph (2), for such State.
“(2) Required use for market stabilization payments to
issuers.–Subject to section 2204(a), an allocation for a State
made pursuant to paragraph (1) for a year shall be used to
carry out the purpose described in section 2202(2) in such
State by providing payments to appropriate entities described
in such section with respect to claims that exceed $50,000 (or,
with respect to allocations made under this title for 2020 or a
subsequent year during the period specified in section 2201,
such dollar amount specified by the Administrator), but do not
exceed $350,000 (or, with respect to allocations made under
this title for 2020 or a subsequent year during such period,
such dollar amount specified by the Administrator), in an
amount equal to 75 percent (or, with respect to allocations
made under this title for 2020 or a subsequent year during such
period, such percentage specified by the Administrator) of the
amount of such claims.
“SEC. 2204. ALLOCATIONS.
“(a) Appropriation.–For the purpose of providing allocations for
States (including pursuant to section 2203(b)) under this title there
is appropriated, out of any money in the Treasury not otherwise
appropriated–
“(1) for 2018, $15,000,000,000;
“(2) for 2019, $15,000,000,000;
“(3) for 2020, $10,000,000,000;
“(4) for 2021, $10,000,000,000;
“(5) for 2022, $10,000,000,000;
“(6) for 2023, $10,000,000,000;
“(7) for 2024, $10,000,000,000;
“(8) for 2025, $10,000,000,000; and
“(9) for 2026, $10,000,000,000.
“(b) Allocations.–
“(1) Payment.–
“(A) In general.–From amounts appropriated under
subsection (a) for a year, the Administrator shall,
with respect to a State and not later than the date
specified under subparagraph (B) for such year,
allocate, subject to subsection (e), for such State
(including pursuant to section 2203(b)) the amount
determined for such State and year under paragraph (2).
“(B) Specified date.–For purposes of subparagraph
(A), the date specified in this subparagraph is–
“(i) for 2018, the date that is 45 days
after the date of the enactment of this title;
and
“(ii) for 2019 and subsequent years,
January 1 of the respective year.
“(2) Allocation amount determinations.–
“(A) For 2018 and 2019.–
“(i) In general.–For purposes of
paragraph (1), the amount determined under this
paragraph for 2018 and 2019 for a State is an
amount equal to the sum of–
“(I) the relative incurred claims
amount described in clause (ii) for
such State and year; and
“(II) the relative uninsured and
issuer participation amount described
in clause (iv) for such State and year.
“(ii) Relative incurred claims amount.–
For purposes of clause (i), the relative
incurred claims amount described in this clause
for a State for 2018 and 2019 is the product
of–
“(I) 85 percent of the amount
appropriated under subsection (a) for
the year; and
“(II) the relative State incurred
claims proportion described in clause
(iii) for such State and year.
“(iii) Relative state incurred claims
proportion.–The relative State incurred claims
proportion described in this clause for a State
and year is the amount equal to the ratio of–
“(I) the adjusted incurred claims
by the State, as reported through the
medical loss ratio annual reporting
under section 2718 of the Public Health
Service Act for the third previous
year; to
“(II) the sum of such adjusted
incurred claims for all States, as so
reported, for such third previous year.
“(iv) Relative uninsured and issuer
participation amount.–For purposes of clause
(i), the relative uninsured and issuer
participation amount described in this clause
for a State for 2018 and 2019 is the product
of–
“(I) 15 percent of the amount
appropriated under subsection (a) for
the year; and
“(II) the relative State uninsured
and issuer participation proportion
described in clause (v) for such State
and year.
“(v) Relative state uninsured and issuer
participation proportion.–The relative State
uninsured and issuer participation proportion
described in this clause for a State and year
is–
“(I) in the case of a State not
described in clause (vi) for such year,
0; and
“(II) in the case of a State
described in clause (vi) for such year,
the amount equal to the ratio of–
“(aa) the number of
individuals residing in such
State who for the third
preceding year were not
enrolled in a health plan or
otherwise did not have health
insurance coverage (including
through a Federal or State
health program) and whose
income is below 100 percent of
the poverty line applicable to
a family of the size involved;
to
“(bb) the sum of the
number of such individuals for
all States described in clause
(vi) for the third preceding
year.
“(vi) States described.–For purposes of
clause (v), a State is described in this
clause, with respect to 2018 and 2019, if the
State satisfies either of the following
criterion:
“(I) The number of individuals
residing in such State and described in
clause (v)(II)(aa) was higher in 2015
than 2013.
“(II) The State have fewer than
three health insurance issuers offering
qualified health plans through the
Exchange for 2017.
“(B) For 2020 through 2026.–For purposes of
paragraph (1), the amount determined under this
paragraph for a year (beginning with 2020) during the
period described in section 2201 for a State is an
amount determined in accordance with an allocation
methodology specified by the Administrator which–
“(i) takes into consideration the adjusted
incurred claims of such State, the number of
residents of such State who for the previous
year were not enrolled in a health plan or
otherwise did not have health insurance
coverage (including through a Federal or State
health program) and whose income is below 100
percent of the poverty line applicable to a
family of the size involved, and the number of
health insurance issuers participating in the
insurance market in such State for such year;
“(ii) is established after consultation
with health care consumers, health insurance
issuers, State insurance commissioners, and
other stakeholders and after taking into
consideration additional cost and risk factors
that may inhibit health care consumer and
health insurance issuer participation; and
“(iii) reflects the goals of improving the
health insurance risk pool, promoting a more
competitive health insurance market, and
increasing choice for health care consumers.
“(c) Annual Distribution of Previous Year’s Remaining Funds.– In
carrying out subsection (b), the Administrator shall, with respect to a
year (beginning with 2020 and ending with 2027), not later than March
31 of such year–
“(1) determine the amount of funds, if any, from the
amounts appropriated under subsection (a) for the previous year
but not allocated for such previous year; and
“(2) if the Administrator determines that any funds were
not so allocated for such previous year, allocate such
remaining funds, in accordance with the allocation methodology
specified pursuant to subsection (b)(2)(B)–
“(A) to States that have submitted an application
approved under section 2203(a) for such previous year
for any purpose for which such an application was
approved; and
“(B) for States for which allocations were made
pursuant to section 2203(b) for such previous year, to
be used by the Administrator for such States, to carry
out the purpose described in section 2202(2) in such
States by providing payments to appropriate entities
described in such section with respect to claims that
exceed $1,000,000;
with, respect to a year before 2027, any remaining funds being
made available for allocations to States for the subsequent
year.
“(d) Availability.–Amounts appropriated under subsection (a) for
a year and allocated to States in accordance with this section shall
remain available for expenditure through December 31, 2027.
“(e) Conditions for and Limitations on Receipt of Funds.–The
Secretary may not make an allocation under this title for a State, with
respect to a purpose described in section 2202–
“(1) in the case of an allocation that would be made to a
State pursuant to section 2203(a), if the State does not agree
that the State will make available non-Federal contributions
towards such purpose in an amount equal to–
“(A) for 2020, 7 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(B) for 2021, 14 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(C) for 2022, 21 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(D) for 2023, 28 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(E) for 2024, 35 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(F) for 2025, 42 percent of the amount allocated
under this subsection to such State for such year and
purpose; and
“(G) for 2026, 50 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(2) in the case of an allocation that would be made for a
State pursuant to section 2203(b), if the State does not agree
that the State will make available non-Federal contributions
towards such purpose in an amount equal to–
“(A) for 2020, 10 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(B) for 2021, 20 percent of the amount allocated
under this subsection to such State for such year and
purpose; and
“(C) for 2022, 30 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(D) for 2023, 40 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(E) for 2024, 50 percent of the amount allocated
under this subsection to such State for such year and
purpose;
“(F) for 2025, 50 percent of the amount allocated
under this subsection to such State for such year and
purpose; and
“(G) for 2026, 50 percent of the amount allocated
under this subsection to such State for such year and
purpose; or
“(3) if such an allocation for such purpose would not be
permitted under subsection (c)(7) of section 2105 if such
allocation were payment made under such section.”.
SEC. 133. CONTINUOUS HEALTH INSURANCE COVERAGE INCENTIVE.
Subpart I of part A of title XXVII of the Public Health Service Act
is amended–
(1) in section 2701(a)(1)(B), by striking “such rate” and
inserting “subject to section 2710A, such rate”;
(2) by redesignating the second section 2709 as section
2710; and
(3) by adding at the end the following new section:
“SEC. 2710A. ENCOURAGING CONTINUOUS HEALTH INSURANCE COVERAGE.
“(a) Penalty Applied.–
“(1) In general.–Notwithstanding section 2701, subject to
the succeeding provisions of this section, a health insurance
issuer offering health insurance coverage in the individual or
small group market shall, in the case of an individual who is
an applicable policyholder of such coverage with respect to an
enforcement period applicable to enrollments for a plan year
beginning with plan year 2019 (or, in the case of enrollments
during a special enrollment period, beginning with plan year
2018), increase the monthly premium rate otherwise applicable
to such individual for such coverage during each month of such
period, by an amount determined under paragraph (2).
“(2) Amount of penalty.–The amount determined under this
paragraph for an applicable policyholder enrolling in health
insurance coverage described in paragraph (1) for a plan year,
with respect to each month during the enforcement period
applicable to enrollments for such plan year, is the amount
that is equal to 30 percent of the monthly premium rate
otherwise applicable to such applicable policyholder for such
coverage during such month.
“(b) Definitions.–For purposes of this section:
“(1) Applicable policyholder.–The term `applicable
policyholder’ means, with respect to months of an enforcement
period and health insurance coverage, an individual who–
“(A) is a policyholder of such coverage for such
months;
“(B) cannot demonstrate (through presentation of
certifications described in section 2704(e) or in such
other manner as may be specified in regulations, such
as a return or statement made under section 6055(d) or
36C of the Internal Revenue Code of 1986), during the
look-back period that is with respect to such
enforcement period, there was not a period of at least
63 continuous days during which the individual did not
have creditable coverage (as defined in paragraph (1)
of section 2704(c) and credited in accordance with
paragraphs (2) and (3) of such section); and
“(C) in the case of an individual who had been
enrolled under dependent coverage under a group health
plan or health insurance coverage by reason of section
2714 and such dependent coverage of such individual
ceased because of the age of such individual, is not
enrolling during the first open enrollment period
following the date on which such coverage so ceased.
“(2) Look-back period.–The term `look-back period’ means,
with respect to an enforcement period applicable to an
enrollment of an individual for a plan year beginning with plan
year 2019 (or, in the case of an enrollment of an individual
during a special enrollment period, beginning with plan year
2018) in health insurance coverage described in subsection
(a)(1), the 12-month period ending on the date the individual
enrolls in such coverage for such plan year.
“(3) Enforcement period.–The term `enforcement period’
means–
“(A) with respect to enrollments during a special
enrollment period for plan year 2018, the period
beginning with the first month that is during such plan
year and that begins subsequent to such date of
enrollment, and ending with the last month of such plan
year; and
“(B) with respect to enrollments for plan year
2019 or a subsequent plan year, the 12-month period
beginning on the first day of the respective plan
year.”.
SEC. 134. INCREASING COVERAGE OPTIONS.
Section 1302 of the Patient Protection and Affordable Care Act (42
U.S.C. 18022) is amended–
(1) in subsection (a)(3), by inserting “and with respect
to a plan year before plan year 2020” after “subsection
(e)”; and
(2) in subsection (d), by adding at the end the following:
“(5) Sunset.–The provisions of this subsection shall not
apply after December 31, 2019, and after such date any
reference to this subsection or level of coverage or plan
described in this subsection and any requirement under law
applying such a level of coverage or plan shall have no force
or effect (and such a requirement shall be applied as if this
section had been repealed).”.
SEC. 135. CHANGE IN PERMISSIBLE AGE VARIATION IN HEALTH INSURANCE
PREMIUM RATES.
Section 2701(a)(1)(A)(iii) of the Public Health Service Act (42
U.S.C. 300gg(a)(1)(A)(iii)), as inserted by section 1201(4) of the
Patient Protection and Affordable Care Act, is amended by inserting
after “(consistent with section 2707(c))” the following: “or, for
plan years beginning on or after January 1, 2018, as the Secretary may
implement through interim final regulation, 5 to 1 for adults
(consistent with section 2707(c)) or such other ratio for adults
(consistent with section 2707(c)) as the State involved may provide”.
TITLE II–COMMITTEE ON WAYS AND MEANS
Subtitle A–Repeal and Replace of Health-Related Tax Policy
SEC. 201. RECAPTURE EXCESS ADVANCE PAYMENTS OF PREMIUM TAX CREDITS.
Subparagraph (B) of section 36B(f)(2) of the Internal Revenue Code
of 1986 is amended by adding at the end the following new clause:
“(iii) Nonapplicability of limitation.–
This subparagraph shall not apply to taxable
years beginning after December 31, 2017, and
before January 1, 2020.”.
SEC. 202. ADDITIONAL MODIFICATIONS TO PREMIUM TAX CREDIT.
(a) Modification of Definition of Qualified Health Plan.–
(1) In general.–Section 36B(c)(3)(A) of the Internal
Revenue Code of 1986 is amended–
(A) by inserting “(determined without regard to
subparagraphs (A), (C)(ii), and (C)(iv) of paragraph
(1) thereof and without regard to whether the plan is
offered on an Exchange)” after “1301(a) of the
Patient Protection and Affordable Care Act”, and
(B) by striking “shall not include” and all that
follows and inserting “shall not include any health
plan that–
“(i) is a grandfathered health plan or a
grandmothered health plan, or
“(ii) includes coverage for abortions
(other than any abortion necessary to save the
life of the mother or any abortion with respect
to a pregnancy that is the result of an act of
rape or incest).”.
(2) Definition of grandmothered health plan.–Section
36B(c)(3) of such Code is amended by adding at the end the
following new subparagraph:
“(C) Grandmothered health plan.–
“(i) In general.–The term `grandmothered
health plan’ means health insurance coverage
which is offered in the individual health
insurance market as of October 1, 2013, and is
permitted to be offered in such market after
January 1, 2014, as a result of CCIIO guidance.
“(ii) CCIIO guidance defined.–The term
`CCIIO guidance’ means the letter issued by the
Centers for Medicare & Medicaid Services on
November 14, 2013, to the State Insurance
Commissioners outlining a transitional policy
for non-grandfathered coverage in the
individual health insurance market, as
subsequently extended and modified (including
by a communication entitled `Insurance
Standards Bulletin Series–INFORMATION–
Extension of Transitional Policy through
Calendar Year 2017′ issued on February 29,
2016, by the Director of the Center for
Consumer Information & Insurance Oversight of
such Centers).
“(iii) Individual health insurance
market.–The term `individual health insurance
market’ means the market for health insurance
coverage (as defined in section 9832(b))
offered to individuals other than in connection
with a group health plan (within the meaning of
section 5000(b)(1)).”.
(3) Conforming amendment related to abortion coverage.–
Section 36B(c)(3) of such Code, as amended by paragraph (2), is
amended by adding at the end the following new subparagraph:
“(D) Certain rules related to abortion.–
“(i) Option to purchase separate coverage
or plan.–Nothing in subparagraph (A) shall be
construed as prohibiting any individual from
purchasing separate coverage for abortions
described in such subparagraph, or a health
plan that includes such abortions, so long as
no credit is allowed under this section with
respect to the premiums for such coverage or
plan.
“(ii) Option to offer coverage or plan.–
Nothing in subparagraph (A) shall restrict any
health insurance issuer offering a health plan
from offering separate coverage for abortions
described in such subparagraph, or a plan that
includes such abortions, so long as premiums
for such separate coverage or plan are not paid
for with any amount attributable to the credit
allowed under this section (or the amount of
any advance payment of the credit under section
1412 of the Patient Protection and Affordable
Care Act).
“(iii) Other treatments.–The treatment of
any infection, injury, disease, or disorder
that has been caused by or exacerbated by the
performance of an abortion shall not be treated
as an abortion for purposes of subparagraph
(A).”.
(4) Conforming amendments related to off-exchange
coverage.–
(A) Advance payment not applicable.–Section 1412
of the Patient Protection and Affordable Care Act is
amended by adding at the end the following new
subsection:
“(f) Exclusion of Off-Exchange Coverage.–Advance payments under
this section, and advance determinations under section 1411, with
respect to any credit allowed under section 36B shall not be made with
respect to any health plan which is not enrolled in through an
Exchange.”.
(B) Reporting.–Section 6055(b) of the Internal
Revenue Code of 1986 is amended by adding at the end
the following new paragraph:
“(3) Information relating to off-exchange premium credit
eligible coverage.–If minimum essential coverage provided to
an individual under subsection (a) consists of a qualified
health plan (as defined in section 36B(c)(3)) which is not
enrolled in through an Exchange established under title I of
the Patient Protection and Affordable Care Act, a return
described in this subsection shall include–
“(A) a statement that such plan is a qualified
health plan (as defined in section 36B(c)(3)),
“(B) the premiums paid with respect to such
coverage,
“(C) the months during which such coverage is
provided to the individual,
“(D) the adjusted monthly premium for the
applicable second lowest cost silver plan (as defined
in section 36B(b)(3)) for each such month with respect
to such individual, and
“(E) such other information as the Secretary may
prescribe.
This paragraph shall not apply with respect to coverage
provided for any month beginning after December 31, 2019.”.
(C) Other conforming amendments.–
(i) Section 36B(b)(2)(A) is amended by
striking “and which were enrolled” and all
that follows and inserting “, or”.
(ii) Section 36B(b)(3)(B)(i) is amended by
striking “the same Exchange” and all that
follows and inserting “the Exchange through
which such taxpayer is permitted to obtain
coverage, and”.
(b) Modification of Applicable Percentage.–Section 36B(b)(3)(A) of
such Code is amended to read as follows:
“(A) Applicable percentage.–
“(i) In general.–The applicable
percentage for any taxable year shall be the
percentage such that the applicable percentage
for any taxpayer whose household income is
within an income tier specified in the
following table shall increase, on a sliding
scale in a linear manner, from the initial
percentage to the final percentage specified in
such table for such income tier with respect to
a taxpayer of the age involved:
————————————————————————————————————————————————————————————————
“In the case of Up to Age 29 Age 30-39 Age 40-49 Age 50-59 Over Age 59
household income —————————————————————————————————————————————————————————-
(expressed as a
percent of the
poverty line)
within the Initial % Final % Initial % Final % Initial % Final % Initial % Final % Initial % Final %
following income
tier:
————————————————————————————————————————————————————————————————
Up to 133% 2…………… 2…………… 2…………… 2………….. 2………….. 2………….. 2………….. 2………….. 2………….. 2
133%-150% 3…………… 4…………… 3…………… 4………….. 3………….. 4………….. 3………….. 4………….. 3………….. 4
150%-200% 4…………… 4.3…………. 4…………… 5.3………… 4………….. 6.3………… 4………….. 7.3………… 4………….. 8.3
200%-250% 4.3…………. 4.3…………. 5.3…………. 5.9………… 6.3………… 8.05……….. 7.3………… 9………….. 8.3………… 10
250%-300% 4.3…………. 4.3…………. 5.9…………. 5.9………… 8.05……….. 8.35……….. 9………….. 10.5……….. 10…………. 11.5
300%-400% 4.3…………. 4.3…………. 5.9…………. 5.9………… 8.35……….. 8.35……….. 10.5……….. 10.5……….. 11.5……….. 11.5
————————————————————————————————————————————————————————————————
“(ii) Age determinations.–
“(I) In general.–For purposes of
clause (i), the age of the taxpayer
taken into account under clause (i)
with respect to any taxable year is the
age attained by such taxpayer before
the close of such taxable year.
“(II) Joint returns.–In the case
of a joint return, the age of the older
spouse shall be taken into account
under clause (i).
“(iii) Indexing.–In the case of any
taxable year beginning in calendar year 2019,
the initial and final percentages contained in
clause (i) shall be adjusted to reflect–
“(I) the excess (if any) of the
rate of premium growth for the period
beginning with calendar year 2013 and
ending with calendar year 2018, over
the rate of income growth for such
period, and
“(II) in addition to any
adjustment under subclause (I), the
excess (if any) of the rate of premium
growth for calendar year 2018, over the
rate of growth in the consumer price
index for calendar year 2018.
“(iv) Failsafe.–Clause (iii)(II) shall
apply only if the aggregate amount of premium
tax credits under this section and cost-sharing
reductions under section 1402 of the Patient
Protection and Affordable Care Act for calendar
year 2018 exceeds an amount equal to 0.504
percent of the gross domestic product for such
calendar year.”.
(b) Effective Date.–
(1) In general.–Except as otherwise provided in this
subsection, the amendments made by this section shall apply to
taxable years beginning after December 31, 2017.
(2) Advance payment not applicable to off-exchange
coverage.–The amendment made by subsection (a)(4)(A) shall
take effect on January 1, 2018.
(3) Reporting.–The amendment made by subsection (a)(4)(B)
shall apply to coverage provided for months beginning after
December 31, 2017.
(4) Modification of applicable percentage.–The amendment
made by subsection (b) shall apply to taxable years beginning
after December 31, 2018.
SEC. 203. PREMIUM TAX CREDIT.
(a) Repeal of Premium Tax Credit.–Section 36B of the Internal
Revenue Code of 1986 is amended by adding at the end the following new
subsection:
“(h) Termination.–No credit shall be allowed under this section
with respect to any coverage month which begins after December 31,
2019.”.
(b) Repeal of Advance Payment of, and Eligibility Determination
for, Premium Tax Credit.–Section 1412 of the Patient Protection and
Affordable Care Act, as amended by the preceding provisions of this
subtitle, is amended by adding at the end the following new subsection:
“(g) Termination With Respect to Premium Tax Credit.–Effective
January 1, 2020, no provision of this section or section 1411 shall
apply to the credit allowed under section 36B of the Internal Revenue
Code of 1986 (or to the advance payment of, or determination of
eligibility for, such credit or payment).”.
(c) Effective Dates.–
(1) Premium tax credit.–The amendment made by subsection
(a) shall apply to months beginning after December 31, 2019, in
taxable years ending after such date.
(2) Eligibility determinations.–The amendment made by
subsection (b) shall take effect on January 1, 2020.
SEC. 204. SMALL BUSINESS TAX CREDIT.
(a) In General.–Section 45R of the Internal Revenue Code of 1986
is amended by adding at the end the following new subsection:
“(j) Shall Not Apply.–This section shall not apply with respect
to amounts paid or incurred in taxable years beginning after December
31, 2019.”.
(b) Disallowance of Small Employer Health Insurance Expense Credit
for Plan Which Includes Coverage for Abortion.–Subsection (h) of
section 45R of the Internal Revenue Code of 1986 is amended–
(1) by striking “Any term” and inserting the following:
“(1) In general.–Any term”; and
(2) by adding at the end the following new paragraph:
“(2) Exclusion of health plans including coverage for
abortion.–
“(A) In general.–The term `qualified health plan’
does not include any health plan that includes coverage
for abortions (other than any abortion necessary to
save the life of the mother or any abortion with
respect to a pregnancy that is the result of an act of
rape or incest) .
“(B) Certain rules related to abortion.–
“(i) Option to purchase separate coverage
or plan.–Nothing in subparagraph (A) shall be
construed as prohibiting any employer from
purchasing for its employees separate coverage
for abortions described in such subparagraph,
or a health plan that includes such abortions,
so long as no credit is allowed under this
section with respect to the employer
contributions for such coverage or plan.
“(ii) Option to offer coverage or plan.–
Nothing in subparagraph (A) shall restrict any
health insurance issuer offering a health plan
from offering separate coverage for abortions
described in such subparagraph, or a plan that
includes such abortions, so long as such
separate coverage or plan is not paid for with
any employer contribution eligible for the
credit allowed under this section.
“(iii) Other treatments.–The treatment of
any infection, injury, disease, or disorder
that has been caused by or exacerbated by the
performance of an abortion shall not be treated
as an abortion for purposes of subparagraph
(A).”.
(c) Effective Dates.–
(1) In general.–The amendment made by subsection (a) shall
apply to taxable years beginning after December 31, 2019.
(2) Disallowance of small employer health insurance expense
credit for plan which includes coverage for abortion.–The
amendments made by subsection (b) shall apply to taxable years
beginning after December 31, 2017.
SEC. 205. INDIVIDUAL MANDATE.
(a) In General.–Section 5000A(c) of the Internal Revenue Code of
1986 is amended–
(1) in paragraph (2)(B)(iii), by striking “2.5 percent”
and inserting “Zero percent”, and
(2) in paragraph (3)–
(A) by striking “$695” in subparagraph (A) and
inserting “$0”, and
(B) by striking subparagraph (D).
(b) Effective Date.–The amendments made by this section shall
apply to months beginning after December 31, 2015.
SEC. 206. EMPLOYER MANDATE.
(a) In General.–
(1) Paragraph (1) of section 4980H(c) of the Internal
Revenue Code of 1986 is amended by inserting “($0 in the case
of months beginning after December 31, 2015)” after
“$2,000”.
(2) Paragraph (1) of section 4980H(b) of the Internal
Revenue Code of 1986 is amended by inserting “($0 in the case
of months beginning after December 31, 2015)” after
“$3,000”.
(b) Effective Date.–The amendments made by this section shall
apply to months beginning after December 31, 2015.
SEC. 207. REPEAL OF THE TAX ON EMPLOYEE HEALTH INSURANCE PREMIUMS AND
HEALTH PLAN BENEFITS.
Section 4980I of the Internal Revenue Code of 1986 is amended by
adding at the end the following new subsection:
“(h) Shall Not Apply.–No tax shall be imposed under this section
with respect to any taxable period beginning after December 31, 2019,
and before January 1, 2025.”.
SEC. 208. REPEAL OF TAX ON OVER-THE-COUNTER MEDICATIONS.
(a) HSAs.–Subparagraph (A) of section 223(d)(2) of the Internal
Revenue Code of 1986 is amended by striking “Such term” and all that
follows through the period.
(b) Archer MSAs.–Subparagraph (A) of section 220(d)(2) of the
Internal Revenue Code of 1986 is amended by striking “Such term” and
all that follows through the period.
(c) Health Flexible Spending Arrangements and Health Reimbursement
Arrangements.–Section 106 of the Internal Revenue Code of 1986 is
amended by striking subsection (f) and by redesignating subsection (g)
as subsection (f).
(d) Effective Dates.–
(1) Distributions from savings accounts.–The amendments
made by subsections (a) and (b) shall apply to amounts paid
with respect to taxable years beginning after December 31,
2017.
(2) Reimbursements.–The amendment made by subsection (c)
shall apply to expenses incurred with respect to taxable years
beginning after December 31, 2017.
SEC. 209. REPEAL OF INCREASE OF TAX ON HEALTH SAVINGS ACCOUNTS.
(a) HSAs.–Section 223(f)(4)(A) of the Internal Revenue Code of
1986 is amended by striking “20 percent” and inserting “10
percent”.
(b) Archer MSAs.–Section 220(f)(4)(A) of the Internal Revenue Code
of 1986 is amended by striking “20 percent” and inserting “15
percent”.
(c) Effective Date.–The amendments made by this section shall
apply to distributions made after December 31, 2017.
SEC. 210. REPEAL OF LIMITATIONS ON CONTRIBUTIONS TO FLEXIBLE SPENDING
ACCOUNTS.
(a) In General.–Section 125 of the Internal Revenue Code of 1986
is amended by striking subsection (i).
(b) Effective Date.–The amendment made by this section shall apply
to taxable years beginning after December 31, 2017.
SEC. 211. REPEAL OF MEDICAL DEVICE EXCISE TAX.
Section 4191 of the Internal Revenue Code of 1986 is amended by
adding at the end the following new subsection:
“(d) Applicability.–The tax imposed under subsection (a) shall
not apply to sales after December 31, 2017.”.
SEC. 212. REPEAL OF ELIMINATION OF DEDUCTION FOR EXPENSES ALLOCABLE TO
MEDICARE PART D SUBSIDY.
(a) In General.–Section 139A of the Internal Revenue Code of 1986
is amended by adding at the end the following new sentence: “This
section shall not be taken into account for purposes of determining
whether any deduction is allowable with respect to any cost taken into
account in determining such payment.”.
(b) Effective Date.–The amendment made by this section shall apply
to taxable years beginning after December 31, 2017.
SEC. 213. REPEAL OF INCREASE IN INCOME THRESHOLD FOR DETERMINING
MEDICAL CARE DEDUCTION.
(a) In General.–Subsection (a) of section 213 of the Internal
Revenue Code of 1986 is amended by striking “10 percent” and
inserting “7.5 percent”.
(b) Extension of Special Rule.–Subsection (f) of section 213 of
such Code is amended–
(1) by striking “2017” and inserting “2018”, and
(2) by striking “and 2016” and inserting “2016, and
2017”.
(c) Effective Date.–
(1) In general.–The amendment made by subsection (a) shall
apply to taxable years beginning after December 31, 2017.
(2) Extension of special rule.–The amendments made by
subsection (b) shall apply to taxable years beginning after
December 31, 2016.
SEC. 214. REPEAL OF MEDICARE TAX INCREASE.
(a) In General.–Subsection (b) of section 3101 of the Internal
Revenue Code of 1986 is amended to read as follows:
“(b) Hospital Insurance.–In addition to the tax imposed by the
preceding subsection, there is hereby imposed on the income of every
individual a tax equal to 1.45 percent of the wages (as defined in
section 3121(a)) received by such individual with respect to employment
(as defined in section 3121(b)).”.
(b) SECA.–Subsection (b) of section 1401 of the Internal Revenue
Code of 1986 is amended to read as follows:
“(b) Hospital Insurance.–In addition to the tax imposed by the
preceding subsection, there shall be imposed for each taxable year, on
the self-employment income of every individual, a tax equal to 2.9
percent of the amount of the self-employment income for such taxable
year.”.
(c) Effective Date.–The amendments made by this section shall
apply with respect to remuneration received after, and taxable years
beginning after, December 31, 2017.
SEC. 215. REFUNDABLE TAX CREDIT FOR HEALTH INSURANCE COVERAGE.
(a) In General.–Subpart C of part IV of subchapter A of chapter 1
of the Internal Revenue Code of 1986 is amended by inserting after
section 36B the following new section:
“SEC. 36C. HEALTH INSURANCE COVERAGE.
“(a) In General.–In the case of an individual, there shall be
allowed as a credit against the tax imposed by this subtitle for the
taxable year the sum of the monthly credit amounts with respect to such
taxpayer for calendar months during such taxable year.
“(b) Monthly Credit Amounts.–
“(1) In general.–The monthly credit amount with respect
to any taxpayer for any calendar month is the lesser of–
“(A) the sum of the monthly limitation amounts
determined under subsection (c) with respect to the
taxpayer and the taxpayer’s qualifying family members
for such month, or
“(B) the amount paid for eligible health insurance
for the taxpayer and the taxpayer’s qualifying family
members for such month.
“(2) Eligible coverage month requirement.–No amount shall
be taken into account under subparagraph (A) or (B) of
paragraph (1) with respect to any individual for any month
unless such month is an eligible coverage month with respect to
such individual.
“(c) Monthly Limitation Amounts.–
“(1) In general.–The monthly limitation amount with
respect to any individual for any eligible coverage month
during any taxable year is \1/12\ of–
“(A) $2,000 in the case of an individual who has
not attained age 30 as of the beginning of such taxable
year,
“(B) $2,500 in the case of an individual who has
attained age 30 but who has not attained age 40 as of
such time,
“(C) $3,000 in the case of an individual who has
attained age 40 but who has not attained age 50 as of
such time,
“(D) $3,500 in the case of an individual who has
attained age 50 but who has not attained age 60 as of
such time, and
“(E) $4,000 in the case of an individual who has
attained age 60 as of such time.
“(2) Limitation based on modified adjusted gross income.–
“(A) In general.–The amount otherwise determined
under subsection (b)(1)(A) (without regard to this
subparagraph but after any other adjustment of such
amount under this section) for the taxable year shall
be reduced (but not below zero) by 10 percent of the
excess (if any) of–
“(i) the taxpayer’s modified adjusted
gross income for such taxable year, over
“(ii) $75,000 (twice such amount in the
case of a joint return).
“(B) Modified adjusted gross income.–For purposes
of this paragraph, the term `modified adjusted gross
income’ means adjusted gross income increased by–
“(i) any amount excluded from gross income
under section 911,
“(ii) any amount of interest received or
accrued by the taxpayer during the taxable year
which is exempt from tax, and
“(iii) an amount equal to the portion of
the taxpayer’s social security benefits (as
defined in section 86(d)) which is not included
in gross income under section 86 for the
taxable year.
“(3) Other limitations.–
“(A) Aggregate dollar limitation.–The sum of the
monthly limitation amounts taken into account under
this section with respect to any taxpayer for any
taxable year shall not exceed $14,000.
“(B) Maximum number of individuals taken into
account.–With respect to any taxpayer for any month,
monthly limitation amounts shall be taken into account
under this section only with respect to the 5 oldest
individuals with respect to whom monthly limitation
amounts could (without regard to this subparagraph)
otherwise be so taken into account.
“(d) Eligible Coverage Month.–For purposes of this section, the
term `eligible coverage month’ means, with respect to any individual,
any month if, as of the first day of such month, the individual–
“(1) is covered by eligible health insurance,
“(2) is not eligible for other specified coverage,
“(3) is either–
“(A) a citizen or national of the United States,
or
“(B) a qualified alien (within the meaning of
section 431 of the Personal Responsibility and Work
Opportunity Reconciliation Act of 1996 (8 U.S.C.
1641)), and
“(4) is not incarcerated, other than incarceration pending
the disposition of charges.
“(e) Qualifying Family Member.–For purposes of this section, the
term `qualifying family member’ means–
“(1) in the case of a joint return, the taxpayer’s spouse,
“(2) any dependent of the taxpayer, and
“(3) with respect to any eligible coverage month, any
child (as defined in section 152(f)(1)) of the taxpayer who as
of the end of the taxable year has not attained age 27 if such
child is covered for such month under eligible health insurance
which also covers the taxpayer (in the case of a joint return,
either spouse).
“(f) Eligible Health Insurance.–For purposes of this section–
“(1) In general.–The term `eligible health insurance’
means any health insurance coverage (as defined in section
9832(b)) if–
“(A) such coverage is either–
“(i) offered in the individual health
insurance market within a State, or
“(ii) is unsubsidized COBRA continuation
coverage,
“(B) such coverage is not a grandfathered health
plan (as defined in section 1251 of the Patient
Protection and Affordable Care Act) or a grandmothered
health plan,
“(C) substantially all of such coverage is not of
excepted benefits described in section 9832(c),
“(D) such coverage does not include coverage for
abortions (other than any abortion necessary to save
the life of the mother or any abortion with respect to
a pregnancy that is the result of an act of rape or
incest),
“(E) such coverage does not consist of short-term
limited duration insurance (as defined by the
Secretary), and
“(F) the State in which such insurance is offered
certifies that such coverage meets the requirements of
this paragraph.
“(2) Rules related to state certification.–
“(A) Certification made available to public.–A
certification shall not be taken into account under
paragraph (1)(E) unless such certification is made
available to the public and meets such other
requirements as the Secretary may provide.
“(B) Special rule for unsubsidized cobra
continuation coverage.–In the case of unsubsidized
COBRA continuation coverage–
“(i) paragraph (1)(E) shall be applied by
substituting `the plan administrator (as
defined in section 414(g)) of the health plan’
for `the State in which such insurance is
offered’, and
“(ii) the requirements of subparagraph (A)
shall be treated as satisfied if the
certification meets such requirements as the
Secretary may provide.
“(3) Grandmothered health plan.–
“(A) In general.–The term `grandmothered health
plan’ means health insurance coverage which is offered
in the individual health insurance market as of January
1, 2013, and is permitted to be offered in such market
after January 1, 2014, as a result of CCIIO guidance.
“(B) CCIIO guidance defined.–The term `CCIIO
guidance’ means the letter issued by the Centers for
Medicare & Medicaid Services on November 14, 2013, to
the State Insurance Commissioners outlining a
transitional policy for non-grandfathered coverage in
the individual health insurance market, as subsequently
extended and modified (including by a communication
entitled `Insurance Standards Bulletin Series–
INFORMATION–Extension of Transitional Policy through
Calendar Year 2017′ issued on February 29, 2016, by the
Director of the Center for Consumer Information &
Insurance Oversight of such Centers).
“(4) Individual health insurance market.–The term
`individual health insurance market’ means the market for
health insurance coverage (as defined in section 9832(b))
offered to individuals other than in connection with a group
health plan (within the meaning of section 5000(b)(1)).
“(g) Other Specified Coverage.–For purposes of this section–
“(1) In general.–The term `other specified coverage’
means any of the following:
“(A) Coverage under a group health plan (within
the meaning of section 5000(b)(1)) other than–
“(i) coverage under a plan substantially
all of the coverage of which is of excepted
benefits described in section 9832(c), and
“(ii) COBRA continuation coverage.
“(B) Coverage under the Medicare program under
part A of title XVIII of the Social Security Act.
“(C) Coverage under the Medicaid program under
title XIX of the Social Security Act.
“(D) Coverage under the CHIP program under title
XXI of the Social Security Act.
“(E) Medical coverage under chapter 55 of title
10, United States Code, including coverage under the
TRICARE program.
“(F) Coverage under a health care program under
chapter 17 or 18 of title 38, United States Code, as
determined by the Secretary of Veterans Affairs, in
coordination with the Secretary of Health and Human
Services and the Secretary of the Treasury.
“(G) Coverage under a health plan under section
2504(e) of title 22, United States Code (relating to
Peace Corps volunteers).
“(H) Coverage under the Nonappropriated Fund
Health Benefits Program of the Department of Defense,
established under section 349 of the National Defense
Authorization Act for Fiscal Year 1995 (Public Law 103-
337; 10 U.S.C. 1587 note).
“(2) Special rule with respect to veterans health
programs.–In the case of other specified coverage described in
paragraph (1)(F), an individual shall not be treated as
eligible for such coverage unless such individual is enrolled
in such coverage.
“(h) Unsubsidized COBRA Continuation Coverage.–For purposes of
this section–
“(1) In general.–The term `unsubsidized COBRA
continuation coverage’ means COBRA continuation coverage no
portion of the premiums for which are subsidized by the
employer.
“(2) COBRA continuation coverage.–The term `COBRA
continuation coverage’ means continuation coverage provided
pursuant to part 6 of subtitle B of title I of the Employee
Retirement Income Security Act of 1974 (other than under
section 609), title XXII of the Public Health Service Act,
section 4980B of the Internal Revenue Code of 1986 (other than
subsection (f)(1) of such section insofar as it relates to
pediatric vaccines), or section 8905a of title 5, United States
Code, or under a State program that provides comparable
continuation coverage. Such term shall not include coverage
under a health flexible spending arrangement.
“(i) Special Rules.–
“(1) Married couples must file joint return.–If the
taxpayer is married (within the meaning of section 7703) at the
close of the taxable year, no credit shall be allowed under
this section to such taxpayer unless such taxpayer and the
taxpayer’s spouse file a joint return for such taxable year.
“(2) Denial of credit to dependents.–
“(A) In general.–No credit shall be allowed under
this section to any individual who is a dependent with
respect to another taxpayer for a taxable year
beginning in the calendar year in which such
individual’s taxable year begins.
“(B) Coordination with rule for older children.–
In the case of any individual who is a qualifying
family member described in subsection (e)(3) with
respect to another taxpayer for any month, in
determining the amount of any credit allowable to such
individual under this section for any taxable year of
such individual which includes such month, the monthly
limitation amount with respect to such individual for
such month shall be zero and no amount paid for
eligible health insurance with respect to such
individual for such month shall be taken into account.
“(3) Coordination with medical expense deduction.–Amounts
described in subsection (b)(1)(B) with respect to any month
shall not be taken into account in determining the deduction
allowed under section 213 except to the extent that such
amounts exceed the amount described in subsection (b)(1)(A)
with respect to such month.
“(4) Insurance which covers other individuals.–For
purposes of this section, rules similar to the rules of section
213(d)(6) shall apply with respect to any contract for eligible
health insurance under which amounts are payable for coverage
of an individual other than the taxpayer and the taxpayer’s
qualifying family members.
“(5) Coordination with advance payments of credit.–With
respect to any taxable year–
“(A) the amount which would (but for this
subsection) be allowed as a credit to the taxpayer
under subsection (a) shall be reduced (but not below
zero) by the aggregate amount paid on behalf of such
taxpayer under section 7529 for months beginning in
such taxable year, and
“(B) the tax imposed by section 1 for such taxable
year shall be increased by the excess (if any) of–
“(i) the aggregate amount paid on behalf
of such taxpayer under section 7529 for months
beginning in such taxable year, over
“(ii) the amount which would (but for this
subsection) be allowed as a credit to the
taxpayer under subsection (a).
“(6) Special rules for qualified small employer health
reimbursement arrangements.–
“(A) In general.–If the taxpayer or any
qualifying family member of the taxpayer is provided a
qualified small employer health reimbursement
arrangement for any eligible coverage month, the sum
determined under subsection (b)(1)(A) with respect to
the taxpayer for such month shall be reduced (but not
below zero) by \1/12\ of the permitted benefit (as
defined in section 9831(d)(3)(C)) under such
arrangement.
“(B) Qualified small employer health reimbursement
arrangement.–For purposes of this paragraph, the term
`qualified small employer health reimbursement
arrangement’ has the meaning given such term by section
9831(d)(2).
“(C) Coverage for less than entire year.–In the
case of an employee who is provided a qualified small
employer health reimbursement arrangement for less than
an entire year, subparagraph (A) shall be applied by
substituting `the number of months during the year for
which such arrangement was provided’ for `12′.
“(7) Certain rules related to abortion.–
“(A) Option to purchase separate coverage or
plan.–Nothing in subsection (f)(1)(D) shall be
construed as prohibiting any individual from purchasing
separate coverage for abortions described in such
subparagraph, or a health plan that includes such
abortions, so long as no credit is allowed under this
section with respect to the premiums for such coverage
or plan.
“(B) Option to offer coverage or plan.–Nothing in
subsection (f)(1)(D) shall restrict any health
insurance issuer offering a health plan from offering
separate coverage for abortions described in such
clause, or a plan that includes such abortions, so long
as premiums for such separate coverage or plan are not
paid for with any amount attributable to the credit
allowed under this section.
“(C) Other treatments.–The treatment of any
infection, injury, disease, or disorder that has been
caused by or exacerbated by the performance of an
abortion shall not be treated as an abortion for
purposes of subsection (f)(1)(D).
“(8) Inflation adjustment.–
“(A) In general.–In the case of any taxable year
beginning in a calendar year after 2020, each dollar
amount in subsection (c)(1), the $75,000 amount in
subsection (c)(2)(A)(ii), and the dollar amount in
subsection (c)(3)(A), shall be increased by an amount
equal to–
“(i) such dollar amount, multiplied by
“(ii) the cost-of-living adjustment
determined under section 1(f)(3) for the
calendar year in which the taxable year begins,
determined–
“(I) by substituting `calendar
year 2019′ for `calendar year 1992′ in
subparagraph (B) thereof, and
“(II) by substituting for the CPI
referred to section 1(f)(3)(A) the
amount that such CPI would have been if
the annual percentage increase in CPI
with respect to each year after 2019
had been one percentage point greater.
“(B) Terms related to cpi.–
“(i) Annual percentage increase.–For
purposes of subparagraph (A)(ii)(II), the term
`annual percentage increase’ means the
percentage (if any) by which CPI for any year
exceeds CPI for the prior year.
“(ii) Other terms.–Terms used in this
paragraph which are also used in section
1(f)(3) shall have the same meanings as when
used in such section.
“(C) Rounding.–Any increase determined under
subparagraph (A) shall be rounded to the nearest
multiple of $50.
“(9) Regulations.–The Secretary may prescribe such
regulations and other guidance as may be necessary or
appropriate to carry out this section, section 6050X, and
section 7529.”.
(b) Advance Payment of Credit; Excess Health Insurance Coverage
Credit Payable to Health Savings Account.–Chapter 77 of such Code is
amended by adding at the end the following:
“SEC. 7529. ADVANCE PAYMENT OF HEALTH INSURANCE COVERAGE CREDIT.
“(a) General Rule.–Not later than January 1, 2020, the Secretary,
in consultation with the Secretary of Health and Human Services, the
Secretary of Homeland Security, and the Commissioner of Social
Security, shall establish a program (hereafter in this section referred
to as the `advance payment program’) for making payments to providers
of eligible health insurance on behalf of taxpayers eligible for the
credit under section 36C.
“(b) Limitation.–The aggregate payments made under this section
with respect to any taxpayer, determined as of any time during any
calendar year, shall not exceed the monthly credit amounts determined
with respect to such taxpayer under section 36C for months during such
calendar year which have ended as of such time.
“(c) Administration.–
“(1) In general.–The advance payment program shall, to
the greatest extent practicable, use the methods and procedures
used to administer the programs created under sections 1411 and
1412 of the Patient Protection and Affordable Care Act
(determined without regard to section 1412(f) of such Act) and
each entity that is authorized to take any actions under the
programs created under such sections (as so determined) shall,
at the request of the Secretary, take such actions to the
extent necessary to carry out this section.
“(2) Application to off-exchange coverage.–Except as
otherwise provided by the Secretary, for purposes of applying
this subsection in the case of eligible health insurance which
is not enrolled in through an Exchange established under title
I of the Patient Protection and Affordable Care Act, the
sections referred to in paragraph (1) shall be applied by
treating references in such sections to an Exchange as
references to the provider of such eligible health insurance
(or, as the Secretary determines appropriate, to the licensed
agent or broker with respect to such insurance), except that
the Secretary of Health and Human Services shall carry out the
responsibilities of the Exchange under section 1411(e)(4) of
the Patient Protection and Affordable Care Act (determined
without regard to section 1412(f) of such Act) in the case of
such insurance.
“(3) Documentation regarding other specified coverage.–
“(A) In general.–The advance payment program
shall provide that any individual applying to have
payments made on their behalf under such program shall,
if such individual (or any qualifying family member of
such individual taken into account in determining the
amount of the credit allowable under section 36C) is
employed, submit a written statement from each employer
of such individual or such qualifying family member
stating whether such individual or qualifying family
member (as the case may be) is eligible for other
specified coverage in connection with such employment.
“(B) Issuance of statements.–An employer shall,
at the request of any employee, provide the statement
under subparagraph (A) at such time, and in such form
and manner, as the Secretary may provide.
“(d) Definitions.–For purposes of this section, terms used in
this section which are also used in section 36C shall have the same
meaning as when used in section 36C.
“SEC. 7530. EXCESS HEALTH INSURANCE COVERAGE CREDIT PAYABLE TO HEALTH
SAVINGS ACCOUNT.
“(a) In General.–At the request of an eligible taxpayer, the
Secretary shall make a payment to the trustee of the designated health
savings account with respect to such taxpayer in an amount equal to the
sum of the excesses (if any) described in subsection (c)(2) with
respect to months in the taxable year.
“(b) Designated Health Savings Account.–The term `designated
health savings account’ means a health savings account of an individual
described in subsection (c)(3) which is identified by the eligible
taxpayer for purposes of this section.
“(c) Eligible Taxpayer.–The term `eligible taxpayer’ means, with
respect to any taxable year, any taxpayer if–
“(1) such taxpayer is allowed a credit under section 36C
for such taxable year,
“(2) the amount described in subparagraph (A) of section
36C(b)(1) exceeds the amount described in subparagraph (B) of
such section with respect to such taxpayer applied with respect
to any month during such taxable year, and
“(3) the taxpayer or one or more of the taxpayer’s
qualifying family members (as defined in section 36C(e)) were
eligible individuals (as defined in section 223(c)(1)) for one
or more months during such taxable year.
“(d) Contributions Treated as Rollovers, etc.–
“(1) In general.–Any amount paid the Secretary to a
health savings account under this section shall be treated for
purposes of this title in the same manner as a rollover
contribution described in section 223(f)(5).
“(2) Coordination with limitation on rollovers.–Any
amount described in paragraph (1) shall not be taken into
account in applying section 223(f)(5)(B) with respect to any
other amount and the limitation of section 223(f)(5)(B) shall
not apply with respect to the application of paragraph (1).
“(e) Form and Manner of Request.–The request referred to in
subsection (a) shall be made at such time and in such form and manner
as the Secretary may provide. To the extent that the Secretary
determines feasible, such request may identify more than one designated
health savings account (and the amount to be paid to each such account)
provided that the aggregate of such payments with respect to any
taxpayer for any taxable year do not exceed the excess described in
subsection (c)(2).
“(f) Taxpayers With Seriously Delinquent Tax Debt.–In the case of
an individual who has a seriously delinquent tax debt (as defined in
section 7345(b)) which has not been fully satisfied–
“(1) if such individual is the eligible taxpayer (or, in
the case of a joint return, either spouse), the Secretary shall
not make any payment under this section with respect to such
taxpayer, and
“(2) if such individual is the account beneficiary (as
defined in section 223(d)(3)) of any health savings account,
the Secretary shall not make any payment under this section to
such health savings account.
“(g) Advance Payment.–To the extent that the Secretary determines
feasible, payment under this section may be made in advance on a
monthly basis under rules similar to the rules of sections 7529 and
36C(i)(5)(B).”.
(c) Information Reporting.–
(1) Reporting by health insurance providers.–Subpart B of
part III of subchapter A of chapter 61 of such Code is amended
by adding at the end the following new section:
“SEC. 6050X. RETURNS BY HEALTH INSURANCE PROVIDERS RELATING TO HEALTH
INSURANCE COVERAGE CREDIT.
“(a) Requirement of Reporting.–Every person who provides eligible
health insurance for any month of any calendar year with respect to any
individual shall, at such time as the Secretary may prescribe, make the
return described in subsection (b) with respect to each such
individual. With respect to any individual with respect to whom
payments under section 7529 are made by the Secretary, the reporting
under subsection (b) shall be made on a monthly basis.
“(b) Form and Manner of Returns.–A return is described in this
subsection if such return–
“(1) is in such form as the Secretary may prescribe, and
“(2) contains, with respect to each policy of eligible
health insurance–
“(A) the name, address, and TIN of each individual
covered under such policy,
“(B) the premiums paid with respect to such
policy,
“(C) the amount of advance payments made on behalf
of the individual under section 7529,
“(D) the months during which such health insurance
is provided to the individual,
“(E) whether such policy constitutes a high
deductible health plan (as defined in section
223(c)(2)), and
“(F) such other information as the Secretary may
prescribe.
“(c) Statements to Be Furnished to Individuals With Respect to
Whom Information Is Required.–Every person required to make a return
under subsection (a) shall furnish to each individual whose name is
required to be set forth in such return a written statement showing–
“(1) the name and address of the person required to make
such return and the phone number of the information contact for
such person, and
“(2) the information required to be shown on the return
with respect to such individual.
The written statement required under the preceding sentence shall be
furnished on or before January 31 of the year following the calendar
year to which such statement relates.
“(d) Definitions.–For purposes of this section, terms used in
this section which are also used in section 36C shall have the same
meaning as when used in section 36C.”.
(2) Reporting by employers.–Section 6051(a) of such Code
is amended by striking “and” at the end of paragraph (14), by
striking the period at the end of paragraph (15) and inserting
“, and”, and by inserting after paragraph (15) the following
new paragraph:
“(16) each month with respect to which the employee is
eligible for other specified coverage (as defined in section
36C(g)) in connection with employment with the employer.”.
(3) Assessable penalties.–
(A) Section 6724(d)(1)(B) of such Code is amended
by striking “or” at the end of clause (xxiv), by
inserting “or” at the end of clause (xxv), and by
inserting after clause (xxv) the following new clause:
“(xxvi) section 6050X (relating to returns
relating to health insurance coverage
credit),”.
(B) Section 6724(d)(2) of such Code is amended by
striking “or” at the end of subparagraph (HH), by
striking the period at the end of subparagraph (II) and
inserting a comma, and by adding after subparagraph
(II) the following new subparagraphs:
“(JJ) section 6050X (relating to returns relating
to health insurance coverage credit), or
“(KK) section 7529(c)(3) (relating to
documentation regarding other specified coverage).”.
(d) Disclosures.–Paragraph (21) of section 6103(l) of the Internal
Revenue Code of 1986 is amended–
(1) in subparagraph (A)–
(A) by striking “any premium tax credit under
section 36B or any cost-sharing reduction under section
1402 of the Patient Protection and Affordable Care Act
or” and inserting “any credit under section 36C”,
(B) by striking “, a State’s children’s health
insurance program under title XXI of the Social
Security Act, or a basic health program under section
1331 of Patient Protection and Affordable Care Act”
and inserting “or a State’s children’s health
insurance program under title XXI of the Social
Security Act”,
(C) by striking “(as defined in section 36B)” in
clause (iv) and inserting “(as defined in section
36C(c)(2)(B))”, and
(D) by striking “or reduction” in clause (v),
(2) in subparagraph (B)–
(A) by striking “may disclose to an Exchange” and
inserting “may disclose–
“(i) to an Exchange”, and
(B) by striking the period at the end and inserting
“, and”, and
(C) by adding at the end the following new clause:
“(ii) in the case of any credit under
section 36C with respect to any health
insurance, the amount of such credit (or the
amount of any advance payment of such credit)
to the provider of such insurance (or, as the
Secretary determines appropriate, the licensed
agent or broker with respect to such
insurance).”, and
(3) in subparagraph (C)(i), by striking “amount of, any
credit or reduction” and inserting “amount of any credit”.
(e) Increased Penalty on Erroneous Claims of Credit.–Section
6676(a) of such Code is amended by inserting “(25 percent in the case
of a claim for refund or credit relating to the health insurance
coverage credit under section 36C)” after “20 percent”.
(f) Conforming Amendments.–
(1) Section 35(g) of such Code is amended by adding at the
end the following new paragraph:
“(14) Coordination with health insurance coverage
credit.–
“(A) In general.–An eligible coverage month to
which the election under paragraph (11) applies shall
not be treated as an eligible coverage month (as
defined in section 36C(d)) for purposes of section 36C
with respect to the taxpayer or any of the taxpayer’s
qualifying family members (as defined in section
36C(e)).
“(B) Coordination with advance payments of health
insurance coverage credit.–In the case of a taxpayer
who makes the election under paragraph (11) with
respect to any eligible coverage month in a taxable
year or on behalf of whom any advance payment is made
under section 7527 with respect to any month in such
taxable year–
“(i) the tax imposed by this chapter for
the taxable year shall be increased by the
excess, if any, of–
“(I) the sum of any advance
payments made on behalf of the taxpayer
under sections 7527 and 7529 for months
during such taxable year, over
“(II) the sum of the credits
allowed under this section (determined
without regard to paragraph (1)) and
section 36C (determined without regard
to subsection (i)(5)(A) thereof) for
such taxable year, and
“(ii) section 36C(i)(5)(B) shall not apply
with respect to such taxpayer for such taxable
year.”.
(2) Section 162(l) of such Code is amended by adding at the
end the following new paragraph:
“(6) Coordination with health insurance coverage credit.–
The deduction otherwise allowable to a taxpayer under paragraph
(1) for any taxable year shall be reduced (but not below zero)
by the sum of–
“(A) the amount of the credit allowable to such
taxpayer under section 36C (determined without regard
to subsection (i)(5)(A) thereof) for such taxable year,
plus
“(B) the aggregate payments made with respect to
the taxpayer under section 7530 for months during such
taxable year.”.
(3) Section 1324(b)(2) of title 31, United States Code is
amended–
(A) by inserting “36C,” after “36B,”, and
(B) by striking “or 6431” and inserting “6431,
or 7530”.
(4) The table of sections for subpart C of part IV of
subchapter A of chapter 1 of the Internal Revenue Code of 1986
is amended by inserting after the item relating to section 36B
the following new item:
“Sec. 36C. Health insurance coverage.”.
(5) The table of sections for subpart B of part III of
subchapter A of chapter 61 of such Code is amended by adding at
the end the following new item:
“Sec. 6050X. Returns by health insurance providers relating to health
insurance coverage credit.”.
(6) The table of sections for chapter 77 of such Code is
amended by adding at the end the following new items:
“Sec. 7529. Advance payment of health insurance coverage credit.
“Sec. 7530. Excess health insurance coverage credit payable to health
savings account.”.
(g) Effective Date.–The amendments made by this section shall
apply to months beginning after December 31, 2019, in taxable years
ending after such date.
SEC. 216. MAXIMUM CONTRIBUTION LIMIT TO HEALTH SAVINGS ACCOUNT
INCREASED TO AMOUNT OF DEDUCTIBLE AND OUT-OF-POCKET
LIMITATION.
(a) Self-Only Coverage.–Section 223(b)(2)(A) of the Internal
Revenue Code of 1986 is amended by striking “$2,250” and inserting
“the amount in effect under subsection (c)(2)(A)(ii)(I)”.
(b) Family Coverage.–Section 223(b)(2)(B) of such Code is amended
by striking “$4,500” and inserting “the amount in effect under
subsection (c)(2)(A)(ii)(II)”.
(c) Conforming Amendments.–Section 223(g)(1) of such Code is
amended–
(1) by striking “subsections (b)(2) and” both places it
appears and inserting “subsection”, and
(2) in subparagraph (B), by striking “determined by” and
all that follows through “`calendar year 2003′.” and
inserting “determined by substituting `calendar year 2003′ for
`calendar year 1992′ in subparagraph (B) thereof .”.
(d) Effective Date.–The amendments made by this section shall
apply to taxable years beginning after December 31, 2017.
SEC. 217. ALLOW BOTH SPOUSES TO MAKE CATCH-UP CONTRIBUTIONS TO THE SAME
HEALTH SAVINGS ACCOUNT.
(a) In General.–Section 223(b)(5) of the Internal Revenue Code of
1986 is amended to read as follows:
“(5) Special rule for married individuals with family
coverage.–
“(A) In general.–In the case of individuals who
are married to each other, if both spouses are eligible
individuals and either spouse has family coverage under
a high deductible health plan as of the first day of
any month–
“(i) the limitation under paragraph (1)
shall be applied by not taking into account any
other high deductible health plan coverage of
either spouse (and if such spouses both have
family coverage under separate high deductible
health plans, only one such coverage shall be
taken into account),
“(ii) such limitation (after application
of clause (i)) shall be reduced by the
aggregate amount paid to Archer MSAs of such
spouses for the taxable year, and
“(iii) such limitation (after application
of clauses (i) and (ii)) shall be divided
equally between such spouses unless they agree
on a different division.
“(B) Treatment of additional contribution
amounts.–If both spouses referred to in subparagraph
(A) have attained age 55 before the close of the
taxable year, the limitation referred to in
subparagraph (A)(iii) which is subject to division
between the spouses shall include the additional
contribution amounts determined under paragraph (3) for
both spouses. In any other case, any additional
contribution amount determined under paragraph (3)
shall not be taken into account under subparagraph
(A)(iii) and shall not be subject to division between
the spouses.”.
(b) Effective Date.–The amendment made by this section shall apply
to taxable years beginning after December 31, 2017.
SEC. 218. SPECIAL RULE FOR CERTAIN MEDICAL EXPENSES INCURRED BEFORE
ESTABLISHMENT OF HEALTH SAVINGS ACCOUNT.
(a) In General.–Section 223(d)(2) of the Internal Revenue Code of
1986 is amended by adding at the end the following new subparagraph:
“(D) Treatment of certain medical expenses
incurred before establishment of account.–If a health
savings account is established during the 60-day period
beginning on the date that coverage of the account
beneficiary under a high deductible health plan begins,
then, solely for purposes of determining whether an
amount paid is used for a qualified medical expense,
such account shall be treated as having been
established on the date that such coverage begins.”.
(b) Effective Date.–The amendment made by this section shall apply
with respect to coverage beginning after December 31, 2017.
Subtitle B–Repeal of Certain Consumer Taxes
SEC. 221. REPEAL OF TAX ON PRESCRIPTION MEDICATIONS.
Section 9008 of the Patient Protection and Affordable Care Act is
amended by adding at the end the following new subsection:
“(l) Termination.–No fee shall be imposed under subsection (a)(1)
with respect to any calendar year beginning after December 31, 2017.”.
SEC. 222. REPEAL OF HEALTH INSURANCE TAX.
Section 9010 of the Patient Protection and Affordable Care Act is
amended by adding at the end the following new subsection:
“(k) Termination.–No fee shall be imposed under subsection (a)(1)
with respect to any calendar year beginning after December 31, 2017.”.
Subtitle C–Repeal of Tanning Tax
SEC. 231. REPEAL OF TANNING TAX.
(a) In General.–The Internal Revenue Code of 1986 is amended by
striking chapter 49.
(b) Effective Date.–The amendment made by this section shall apply
to services performed after December 31, 2017.
Subtitle D–Remuneration From Certain Insurers
SEC. 241. REMUNERATION FROM CERTAIN INSURERS.
Paragraph (6) of section 162(m) of the Internal Revenue Code of
1986 is amended by adding at the end the following new subparagraph:
“(I) Termination.–This paragraph shall not apply
to taxable years beginning after December 31, 2017.”.
Subtitle E–Repeal of Net Investment Income Tax
SEC. 251. REPEAL OF NET INVESTMENT INCOME TAX.
(a) In General.–Subtitle A of the Internal Revenue Code of 1986 is
amended by striking chapter 2A.
(b) Effective Date.–The amendment made by this section shall apply
to taxable years beginning after December 31, 2017.
Union Calendar No. 30
115th CONGRESS
1st Session
H. R. 1628
[Report No. 115-52]
_______________________________________________________________________
A BILL
To provide for reconciliation pursuant to title II of the concurrent
resolution on the budget for fiscal year 2017.
_______________________________________________________________________
March 20, 2017
Committed to the Committee of the Whole House on the State of the Union
and ordered to be printed